Report to Congress
on Activities Related to Autism Spectrum Disorder and Other Developmental Disabilities
FY 2019 - FY 2023
Required Elements

Required Elements of the Report to Congress
(FY 2019 – FY 2023)
In addition to a summary of the roles of the IACC and the NAC in coordinating federal autism-related efforts, this Report to Congress provides an overview of each federal agency that supports projects or programs related to autism, as well as information on current autism prevalence estimates; the present diagnostic and interventions landscape; ongoing efforts in autism supports and services, including home- and community-based services and supports; and progress on implementation of the IACC Strategic Plan.
With data from over 25 federal departments, agencies, divisions, and offices, this report addresses autism research and services according to the required elements outlined in the Autism CARES Act of 2019 [see Report to Congress (FY 2019 – FY 2023) section on page 5 for a complete list of required elements]. Elements (A) and (B) have been combined into one chapter covering the general progress made and amounts expended during the past five years in autism efforts by federal departments, agencies, divisions, and offices. Elements (G) and (H) have been combined into one chapter covering the effectiveness and outcomes of existing and newly developed interventions for individuals on the autism spectrum.
The following federal departments and agencies are included in this report:
- Department of Health and Human Services (HHS)
- Administration for Children and Families (ACF)
- Administration for Community Living (ACL)
- Administration for Strategic Preparedness & Response (ASPR)*
- Agency for Healthcare Research and Quality (AHRQ)
- Centers for Disease Control and Prevention (CDC)
- Centers for Medicare & Medicaid Services (CMS)
- Food and Drug Administration (FDA)
- Health Resources and Services Administration (HRSA)
- Indian Health Service (IHS)
- National Institutes of Health (NIH)
- Office of the Assistant Secretary for Planning and Evaluation (ASPE)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Department of Defense (DoD)
- Department of Education (ED)
- Department of Housing and Urban Development (HUD)
- Department of Justice (DOJ)
- Department of Labor (DOL)
- Department of Transportation (DOT)
- Department of Veterans Affairs (VA)
- Environmental Protection Agency (EPA)
- Institute of Museum and Library Services (IMLS)*
- National Aeronautics and Space Administration (NASA)*
- National Endowment for the Arts (NEA)*
- National Science Foundation (NSF)
- Social Security Administration (SSA)
- U.S. Agency for International Development (USAID)*
- U.S. Geological Survey (USGS)*
* Departments and agencies with an asterisk are those appearing for the first time in this report and have not previously been mentioned in prior reports to Congress on federal autism activities.
Autism Progress and Expenditures
This portion of the report covers Section 399DD(a)(2)(A) and (B) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which require: (A) "A description of the progress made in implementing the provisions of the Autism CARES Act of 2019" and (B) "A description of the amounts expended on the implementation of the amendments made by the Autism CARES Act of 2019." In accordance with the statute, details are provided from the agencies, divisions, and offices within HHS that are involved in autism research and services activities, including ACF, ACL, ASPR, AHRQ, CDC, CMS, FDA, HRSA, ASPE, IHS, NIH, and SAMHSA, as well as from DoD, ED, HUD, DOJ, DOL, DOT, VA, EPA, IMLS, NASA, NEA, NSF, SSA, USAID, and USGS.
Department of Health and Human Services (HHS)
The mission of the U.S. Department of Health and Human Services (HHS) is to enhance and protect the health and well-being of all Americans by providing effective health and human services and fostering advances in medicine, public health, and social services. HHS includes more than 300 programs and 11 operating divisions covering a wide spectrum of activities. The HHS offices and agencies represented in this report support research and services that address the needs of individuals on the autism spectrum and their families and/or individuals with disabilities more broadly.
Administration for Children and Families (ACF)
The Administration for Children and Families (ACF) promotes the economic and social well-being of families, children, individuals, and communities. ACF programs aim to:
- Empower families and individuals to increase their economic independence and productivity;
- Encourage strong, healthy, supportive communities to have a positive impact on quality of life and the development of children;
- Improve access to services through planning, reform, and integration;
- Create partnerships with front-line service providers, states, localities, and tribal communities to identify and implement solutions that transcend traditional program boundaries; and
- Address the needs, strengths, and abilities of vulnerable populations, including people with developmental disabilities, refugees, and migrants.
The ACF does not have any programs or funding specifically focused on provisions of the Autism CARES Act of 2019. However, ACF funds several offices and projects that support inclusion of young children with disabilities, including those with ASD.
The ACF Office of Head Start (OHS) promotes the school readiness of children ages birth to 5 from low-income families by enhancing their cognitive, social, and emotional development. The Head Start programs, authorized under the Head Start Act, as amended, enroll nearly one million age- and income-eligible children nationwide in a typical year. Head Start programs are required to ensure that at least 10% of slots are occupied by children eligible for services under the Individuals with Disabilities Education Act (IDEA). While some children enter Head Start with a diagnosis of a disability, all enrolled children from birth to age 5 are required to receive a developmental screening and, if warranted, are referred for formal evaluation to assess eligibility for services under the IDEA. Furthermore, the Head Start Program Performance Standards outline the requirements that all Head Start agencies that provide services to children and families must meet. This includes requirements for services to children with disabilities, requirements for services to parents of children with disabilities, and requirements to coordinate and collaborate with the local agency responsible for implementing IDEA. Many IDEA, Part B, and IDEA, Part C, services, including early intervention services, and special education and related services are provided through children’s Head Start enrollment.
According to the 2019 Head Start Program Information Report, 0.53% of Head Start’s total enrollment were children diagnosed with ASD. These children and their families received Head Start’s comprehensive services in inclusive settings. The OHS Training and Technical Assistance Centers carry out significant work and activities that promote inclusion of children with disabilities, including those with ASD who are served in Early Head Start and Head Start settings. OHS maintains the Head Start Center for Inclusion website, which offers a variety of resources that support early childhood educators to ensure that children with disabilities can participate as full members of their learning communities. OHS also maintains the disabilities services section of the Early Childhood Learning and Knowledge Center website, which includes evidence-based resources that promote early identification, referrals, family support services, cross-agency collaboration, and resources related to access and full participation of young children with disabilities in inclusive learning environments.
The ACF Office of Planning, Research, and Evaluation (OPRE) studies ACF programs and the populations they serve through rigorous research and evaluation projects. These include evaluations of existing programs, evaluation of innovative approaches to help low-income children and families, research syntheses, and descriptive and exploratory studies. OPRE is currently conducting the Study of Disability Services Coordinators and Inclusion in Head Start (2019-2024) that will provide a descriptive national picture of the Disability Services Coordinators workforce for Early Head Start and Head Start, including American Indian and Alaska Native (Region XI) and Migrant and Seasonal Head Start (Region XII) grantees. It will also explore practices and policies for working with staff, families, children, and the community. This effort will explore how Early Head Start and Head Start serve children with disabilities and their families and will seek to understand how Early Head Start and Head Start collaborate with services in the community, including health providers, Local Education Agencies, and IDEA, Part C.
OPRE is also conducting the Family and Childhood Experiences (FACES; 1997-2026) study to provide descriptive, nationally representative information on preschool-aged children in Head Start in Regions I-X, and American Indian and Alaska Native FACES provides representative information for Head Start in Region XI, including the characteristics, experiences, and development of children and their families and the characteristics of the Head Start programs and staff who serve them. This study collects information on whether children have a disability, what type of disability (autism is grouped into the cognitive disability category), whether the children have multiple disabilities, and how many children with a disability have an Individualized Education Plan (IEP) or Individualized Family Service Plan (IFSP). Likewise, the Early Head Start Family and Children Experiences Survey (Baby FACES; 2009-2023) reports on the percentage of children in Early Head Start programs in Regions I-X that have any special needs, the type of special needs (e.g., developmental disability or delay), and the percentage of children with an IFSP.
ACF maintains the Autism Awareness and Acceptance in Early Childhood Education webpage, which focuses on providing information on ASD to early childhood educators. The webpage includes fact sheets, helpful tips, advice on finding local resources, and links to multiple relevant websites. The tip sheets, compiled by ACF and the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), NIH, contain numerous strategies suggested by experts from across the country for working with children with ASD.
In addition to the ASD webpage, ACF has focused its attention on developmental and behavioral screening. While the emphasis of this priority is broad screening, rather than screening for specific disorders, the initiative has helped inform the early childhood field and ultimately helps children with all disabilities, including those with ASD.
While ACF does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by ACF are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. ACF activities are also relevant to Question 1 (Screening and Diagnosis), Question 4 (Interventions), and Question 5 (Services and Supports) of the IACC Strategic Plan. ACF is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Table 4: ACF Head Start expenditure for children with ASD, FY 2019 – FY 2022
| ACF Head Start ASD-Related Expenditures: FY 2019 – FY 2022 | |
|---|---|
| Fiscal Year | Expenditures |
Fiscal Year2019 |
Expenditures$38 million |
Fiscal Year2020 |
Expenditures$44 million |
Fiscal Year2021 |
Expenditures$49 million |
Fiscal Year2022 |
Expenditures$67 million |
FY 2023 data was not available at the time this report was written.
Administration for Community Living (ACL)
The Administration for Community Living (ACL) works to increase access to community support systems for older adults and people with disabilities. ACL was created around the fundamental principle that older adults and people of all ages with disabilities should be able to live where they choose, with the people they choose, and with the ability to participate fully in their communities. ACL funds programs in all states and territories that support individuals with disabilities, including individuals with autism, living in the community.
Projects of National Significance (PNS), authorized under the Developmental Disabilities Assistance and Bill of Rights Act (Public Law 106-402), focus on the most pressing issues affecting people with developmental disabilities and their families, creating and enhancing opportunities for these individuals to contribute to, and participate in, all facets of community life. Through PNS, ACL’s Administration on Disabilities (AoD) supports the development of national and state policy and awards grants and contracts that enhance the independence, productivity, inclusion, and integration of people with developmental disabilities. Current projects funded under PNS are listed below.
- The State of the States in Intellectual and Developmental Disabilities Project is a comparative nationwide longitudinal study of public programs, funding, and trends in developmental disabilities services and supports. The website includes a "create a chart" feature, allowing the public to analyze and compare data.
- The Empowering Youth with Intellectual and Developmental Disabilities to Manage Their Healthcare Transitions project is a five-year grant started in FY 2021 to establish a national, person-centered, culturally competent resource center to empower youth with intellectual and developmental disabilities in directing their own health care transitions from pediatric to adult models of care. The center is working to increase self-determination, independence, and quality of life for youth with intellectual and developmental disabilities as they transition into adult models of care. Project activities include a national community of practice, co-led by members of the resource center’s Youth Steering Committee, and a mobile app designed for youth with intellectual and developmental disabilities to use during health care transitions. Anticipated outcomes of this initiative include youth with intellectual and developmental disabilities leading their medical appointments and interactions with medical professionals; leading their at-home health care routines such as medication management; making decisions about their health care and wellness next steps, in consultation with providers, family members, and adult guardians; and learning how to proactively manage potential co-occurring health conditions.
- The Self-Advocacy Resource and Technical Assistance Center (SAR-TAC) is a five-year grant started in FY 2021 to establish a national, person-centered, culturally competent resource that empowers and supports the national self-advocacy movement for people with intellectual and developmental disabilities. This center serves as a national resource that further strengthens statewide and local self-advocacy organizations, creates and disseminates self-advocacy resources, provides leadership development opportunities for people with intellectual and developmental disabilities, and strengthens the network of civil rights organizations working on behalf of people with intellectual and developmental disabilities. SAR-TAC is guided by principles of independent living, self-determination, and intersectionality. An advisory committee comprised entirely of people with intellectual and developmental disabilities guides the work of SAR-TAC.
- The Center for Youth Voice, Youth Choice (CYVYC) is a five-year initiative, started in FY 2020, that created a resource center on alternatives to guardianship for youth with intellectual and developmental disabilities. CYVYC developed a national coalition of stakeholders that endorse and share information about alternatives to guardianship and conduct research on the policies and practices related to guardianship and its alternatives. The Youth Ambassador program provides support, mentorship, and leadership development to youth with intellectual and developmental disabilities who will serve on advisory boards and as resource contacts in their states. An expected outcome of the initiative is that fewer youth are subject to guardianship.
- The Disability Employment Technical Assistance Center is a five-year project started in FY 2020. The Center provides tools and resources to ACL disability-focused grantees so that they may more effectively help individuals with disabilities, including autism, achieve meaningful employment with competitive wages in integrated settings. The Center maximizes knowledge transfer across programs by identifying and providing training on innovative, promising, and emerging practices. Expected outcomes include improvements in competitive integrated employment and economic status for individuals with an array of disabilities.
- The Direct Care Workforce Strategies Center is a five-year grant funded in FY 2022 to establish a national center to expand and strengthen the direct care workforce across the country. When fully operational, the Center will serve as a hub, providing tools, resources, and training to assist state systems and service providers and to support the development and coordination of policies and programs that contribute to a stable, robust direct care workforce. The Center’s website will share resources from the federal government, highlight state and local model policies and best practices that can be replicated or adapted, training, and technical assistance materials. In addition, the Center will facilitate peer-to-peer sharing of lessons learned and promising practices through learning collaboratives and support collaboration between state systems, including Medicaid, aging, disability, and workforce agencies; service providers; and aging, disability, and labor stakeholders.
- The National Resource Center for Persons with Intellectual and Developmental Disabilities and Co-Occurring Mental Health and Related Conditions, awarded in FY 2022, will create a national, person-centered, culturally competent resource center to increase access to supports for individuals with intellectual and developmental disabilities and mental health support needs. The objectives of this project are to create a center that will provide an opportunity to elevate best practices in policy, clinical, and workforce capacity while improving the engagement of individuals with disabilities and their families in identifying effective treatment and support services. Additional project partners include the Nisonger Center at Ohio State University, the Autistic Self Advocacy Network, Green Mountain Self Advocates, the Sonoran Center, Center for Systemic Therapeutic Assessment, Resources and Treatment Services, and Communication First. Project activities include Hosted Shared Learning Groups through quarterly virtual gatherings focused on individuals with co-occurring intellectual and developmental disabilities and mental health disabilities, families, state system leaders, and professionals. Expected outcomes include development of effective, equitable, understandable, and respectful quality care and services that are responsive to diverse cultural beliefs and practices, preferred languages, and communication strategies (including the use of alternative augmentative communication), health literacy, and other needs, designed to increase self-determination, empowerment, and quality of life for people with co-occurring intellectual and developmental disabilities and mental health conditions.
ACL has programs to support caregivers, including the National Family Caregiver Support Program and the Lifespan Respite Care Program. ACL also manages the RAISE (Recognize, Assist, Include, Support, and Engage) Family Caregiving Advisory Council (FCAC), which was created under the RAISE Family Caregivers Act of 2018 to advise the HHS Secretary on effective models of both family caregiving and support to family caregivers. The RAISE Family Caregivers Act directs the HHS Secretary to convene the FCAC, deliver a report to Congress, and develop a national family caregiving strategy. The FCAC released their first Report to Congress in 2021. The report describes the current landscape of family caregiving and provides 26 recommendations for how the federal government, states, tribes, territories, and communities can partner with the private sector to better support family caregivers. The 2022 National Strategy to Support Family Caregivers was released in September 2022. It identifies more than 500 actions that communities, providers, government, and others can take to better recognize and support family caregivers. The Strategy also addresses four key principles that must be reflected in all efforts to improve the recognition, assistance, and inclusion of family caregivers and those they support.
The National Institute on Disability, Independent Living, and Rehabilitation Research (NIDILRR) within ACL conducts research and development in disability and rehabilitation, including research and development in ASD, as authorized by the Workforce Innovation and Opportunity Act (WIOA), 45 CFR Part 1330. Research in autism currently funded by NIDILRR is field initiated (i.e., the projects were developed and proposed by researchers in the field).
Additional ACL programs that support community living are described in the Effectiveness and Outcomes of Interventions section of the report on page 105.
While ACL does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by ACL are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve health, well-being, and community living opportunities, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. Research and services activities funded by ACL additionally support Question 4 (Interventions), Question 5 (Services and Supports), and Question 6 (Lifespan) of the IACC Strategic Plan. ACL is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Administration for Strategic Preparedness & Response (ASPR)
The Administration for Strategic Preparedness & Response (ASPR) is an operating division within HHS that leads the nation’s medical and public health preparedness for, response to, and recovery from disasters and other public health emergencies. ASPR collaborates with hospitals; health care coalitions; biotech firms; community members; state, local, tribal, and territorial governments; and other partners across the country to improve readiness and response capabilities. ASPR continues to evolve to be even better prepared to address future health threats and protect national health security.
While not limited to autism, HHS/ASPR recently published the new HHS Child and Adolescent Health Emergency Planning Toolkit: Guidance for Addressing the Needs of Children and Youth with Special Health Care Needs. Development of this guidance was a joint project of the ASPR At-Risk Individuals Program and HRSA’s Maternal and Child Health Bureau. This toolkit addresses the needs of children and youth with special health care needs (CYSHCN), including children and youth with autism and children and youth at increased risk for other chronic physical, neurological, developmental, behavioral, or emotional conditions who require health and other services beyond those required by children or youth generally, and their families and caregivers. The toolkit is designed to improve the capacity of health care, public health, and social services professionals and emergency managers in addressing the needs of CYSHCN in emergency preparedness, response, recovery, mitigation, and community resilience activities. Partnering CYSHCN and their families and caregivers with health care providers and public health and social services professionals can reduce the heavy burden of emergency planning that often falls on families and caregivers. The toolkit outlines basic planning steps, highlights key resources and promising practices, and explains data and information to be integrated into emergency planning for CYSHCN. It includes modules on preparedness, response, and recovery planning, and a module with case studies covering three emergency scenarios. Throughout, the toolkit promotes understanding of health equity and applying the social determinants of health, developing organizational resilience, and understanding the needs of CYSHCN populations before, during, and after emergencies.
ASPR also manages the National Advisory Committee on Individuals with Disabilities and Disasters (NACIDD). NACIDD evaluates issues and programs and provides findings, advice, and recommendations to the HHS Secretary and ASPR to support and enhance all-hazards public health and medical preparedness, response, and recovery activities related to meeting the needs of individuals with disabilities, including individuals on the autism spectrum. In addition to the NACIDD, ASPR manages the National Advisory Committee on Children and Disasters (NACCD). The NACCD recently issued recommendations to HHS and ASPR regarding the mental health of children that consider the vulnerabilities of children with disabilities and other special health care needs that should be incorporated in disaster preparedness, response, and recovery activities to promote resilience.
While ASPR does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by ASPR are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. ASPR activities are relevant to Question 5 (Services and Supports) and Question 6 (Lifespan) of the IACC Strategic Plan.
Agency for Healthcare Research and Quality (AHRQ)
The mission of the Agency for Healthcare Research and Quality (AHRQ) is to produce evidence to make health care safer, higher quality, more accessible, equitable, and affordable and to work within HHS and with other partners to make sure that the evidence is understood and used. AHRQ does not receive funds from the Autism CARES Act of 2019 but does support research to determine the effectiveness and outcomes of interventions for individuals with ASD. This is achieved through funding extramural investigator-initiated research, promoting the development of practice improvement tools that apply and use the latest scientific evidence in advancing care delivery, and using data and analytics to evaluate health and health care, in line with the Agency’s mission. Some of these programs and research projects are described below, and further details can be found on the AHRQ website.
The mission of AHRQ’s Digital Healthcare Research Program is to produce and disseminate evidence about how the evolving digital health care ecosystem can best advance the quality, safety, and effectiveness of health care for patients and their families. The program provides foundational research to ensure that digital health care systems are designed and implemented in ways that improve quality and safety, while not resulting in excessive burden on physicians and other members of the care team. Current research areas include usability, consumer-focused digital health care, clinical decision support, safety, patient-reported outcomes, and care transitions.
Since 1998, AHRQ has been authorized by Congress to convene and provide ongoing scientific, administrative, and dissemination support to the U.S. Preventive Services Task Force (USPSTF). The USPSTF is an independent volunteer panel of national experts in prevention and evidence-based medicine. The Task Force works to improve the health of people nationwide by making evidence-based recommendations about clinical preventive services such as screenings, counseling services, and preventive medications. All recommendations are published on the USPSTF website and/or in peer-reviewed journals. Task Force members come from the fields of preventive medicine and primary care, including internal medicine, family medicine, pediatrics, behavioral health, obstetrics and gynecology, and nursing. Their recommendations are based on a rigorous review of existing peer-reviewed evidence and are intended to help primary care clinicians and patients decide together whether a preventive service is right for a patient’s needs. Each year, the Task Force makes a report to Congress that identifies critical evidence gaps in research related to clinical preventive services and recommends priority areas that deserve further examination. More information on these reports is available on the USPSTF website.
In June 2021, USPSTF posted the final research plan regarding screening for ASD in young children. This project is currently in progress and addresses the following key questions:
- Does screening for ASD in children ages 12 to 36 months improve:
- Access and timing of ASD evaluation, diagnosis, and intervention?
- Developmental, functional, and quality of life outcomes?
- What is the accuracy of screening instruments to detect ASD in children ages 12 to 36 months?
- What are the harms of screening for ASD in children ages 12 to 36 months and their families?
- Do interventions targeting young children with ASD improve developmental, functional, and quality of life outcomes? To what extent is the timing of intervention initiation (by age and in relation to the establishment of an ASD diagnosis) associated with ASD-related outcomes?
- What are the harms of interventions for ASD in young children?
The Evidence-Based Practice Center Program reviews and synthesizes published and unpublished scientific information for use by clinicians, health systems, and policymakers in health care decision-making. Stakeholders are involved throughout the research process to improve research results and ensure findings are relevant to users’ distinct concerns. Previous reports on autism are listed in the Autism Spectrum Disorder webpage.
The Medical Expenditure Panel Survey (MEPS) is a set of large-scale surveys of families and individuals, their medical providers, and employers across the United States. MEPS is the most complete source of data on the cost and use of health care and health insurance coverage.
As a collaboration among the University of California, Los Angeles, Kaiser Permanente Southern California, the VA Greater Los Angeles Healthcare System, and the Los Angeles County Department of Health Services, the Stakeholder-Partnered Implementation Research and Innovation Translation (SPIRIT) program, awarded under the AHRQ and Patient-Centered Outcomes Research Institute Institutional Mentored Career Development Program (K12), is designed to prepare outstanding postdoctoral scholars for academic research careers focused on rapid and sustainable uptake of new scientific discoveries and innovations that improve the design, delivery, and outcomes of care for chronic diseases at the individual, population, and health care system levels. A supplement to the SPIRIT K12 Program, PA-20-072 Stakeholder-Partnered Implementation Research and Innovation Translation (SPIRIT) Program: Vulnerable Populations Cared for by Learning Health Systems During the COVID-19 Pandemic (K12HS026407), leveraged existing K12 Scholar projects and expanded the specific aims of their ongoing research to develop high-impact new knowledge concerning the COVID-19 pandemic. Three K12 scholars proposed supplemental work that addressed health issues that arose due to COVID-19. These projects addressed how different vulnerable populations with health care needs, including children with ASD, managed during the stay-at-home orders of the COVID-19 pandemic and evaluated their experiences with telehealth during stay-at-home orders.
AHRQ researchers contributed to two manuscripts published in 2021 addressing the cost and use of health care and health insurance coverage among families and children with ASD. One study used data from 2003 to 2015 for children ages 3-17 years in the MEPS linked to the National Health Interview Survey (NHIS) Sample Child Core questionnaire.7 The study found the incremental annual per-child cost of ASD relative to no ASD diagnosis was $3,930 (2018 U.S. dollars) using ASD case status from the NHIS Child Core questionnaire and $5,621 using current-year ASD case status from MEPS. Both estimates are lower than some published estimates but still represent substantial costs to the U.S. health care system.
The second study estimated changes in spending among privately insured children with and without current ASD using 2011-2017 claims data from employer-sponsored health plans for children ages 3-7.8 The study found that mean spending per child with a current-year ASD diagnosis increased by 51% in 2017 U.S. dollars, from roughly $13,000 in 2011 to $20,000 in 2017. Among children who did not meet the current-year ASD case definition, per-child spending increased by 8%. Spending on children with ASD accounted for 41% of spending growth for children ages 3-7 during 2011-2017. Outpatient behavioral intervention-related spending per child with ASD increased by 376%, from $1,746 in 2011 to $8,317 in 2017; spending on all other services increased by 2%. The share of behavioral intervention-related spending increased from 13% in 2011 to 42% in 2017. In 2011, 2.5% of children with current-year ASD diagnoses incurred $20,000 in outpatient behavioral intervention-related spending, which increased to 14.4% in 2017. Overall, during 2011-2017, spending increased six times as much for privately insured children ages 3-7 with current-year ASD as for children without ASD, largely from increased behavioral intervention-related spending, with one in seven children receiving at least $20,000 in services in 2017.
Additional AHRQ-funded projects focused on the effectiveness and outcomes of interventions are described on page 107.
While AHRQ does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, research conducted and funded by AHRQ are relevant to individuals with disabilities, including those on the autism spectrum and their families. AHRQ funds research that address Question 1 (Screening and Diagnosis), Question 4 (Interventions), Question 5 (Services and Supports), and Question 7 (Infrastructure and Prevalence) of the IACC Strategic Plan. AHRQ is a member of the IACC and the FIWA and participates in efforts to coordinate autism activities across the federal government.
Centers for Disease Control and Prevention (CDC)
The Centers for Disease Control and Prevention (CDC) is the nation’s leading science-based, data-driven service agency that protects the public’s health. CDC brings a unique public health perspective to the effort to understand ASD and offers resources to the community. CDC is committed to providing essential data on ASD, searching for factors that put children at risk for ASD and possible causes, and developing resources that help identify children with ASD as early as possible. The Autism CARES Act of 2019 reauthorized CDC’s autism-related work for a further five years and called for a surveillance and research program with a focus across the lifespan and to address health disparities. CDC has continued expansion to explore ASD in diverse communities, better track early identification, and understand the transition to adolescence and adulthood.
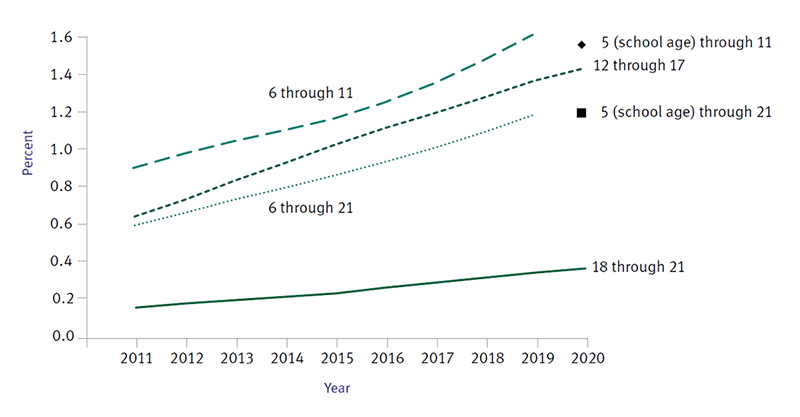
Established in 2000, the ADDM Network is the only network to track the number and characteristics of children with autism and other developmental disabilities in multiple communities throughout the United States. In 2020, 2021, and 2023, CDC released reports that provide the number and characteristics of children with ASD and how early they are identified.1,9,10 These data are used for national, state, and local policy and planning.
In 2019, the ADDM Network began implementing a new case definition and data system which had multiple advantages over the previous method. The simplified methods required fewer resources and allowed for more efficient data collection. The 2023 prevalence report was published a full year faster than the previous method would have allowed. The ADDM Network was also able to expand its tracking of early ASD identification among children aged 4.3,11,12 Previously, six of 11 ADDM sites were able to conduct early identification surveillance among 4-year-olds in only a portion of their study area; for surveillance years 2018 and 2020, all 11 sites reported early identification information for their full study area, tripling the population for this important indicator. Surveillance among 4-year-olds is important because early identification of ASD is the best way to ensure children get necessary services and supports to reach their full potential. In addition to expanding to younger ages, the ADDM Network was also able to collect and report data on children aged 16 years with ASD in five ADDM sites, marking an expansion of ASD surveillance to help communities identify health care needs and gaps in planning for the transition to adulthood among youth with ASD.
The new ADDM data system was also able to scale to statewide datasets to provide state- and county-level information in a pilot study.13 The study found that linking statewide health and education data is an effective way for states to have actionable local ASD prevalence estimates when resources are limited. In addition, the ADDM Network was well positioned to report how the new Lancet Commission’s proposed term "profound autism" might apply to its surveillance population, as ADDM sites have tracked the number and characteristics of young children with ASD across multiple diverse communities in the United States for over 20 years. CDC released a report assessing the number of 8-year-old children in the ADDM Network from 2000–2016 who met the newly-proposed profound autism definition and how they compared to 8-year-old children with autism who did not meet the definition over this period.14
In April 2023, with support from the Consolidated Appropriations Act, 2023, ADDM expanded from 11 to 16 sites across the United States, with nine ADDM sites now tracking transition planning and co-occurring conditions among 16-year-old children with ASD. Data for new sites will be included for the 2022 surveillance year.
CDC continues to maintain and update its Autism Data Visualization Tool that lets users explore available data on the prevalence, demographics, and other characteristics of children with ASD from four federal data sources: ADDM Network, ED Special Education Child Count, Medicaid, and National Survey of Children’s Health (NSCH). The website was launched in April 2019 and has garnered over 145,000 page views as of September 2023. This tool provides an easy way to access national, state, and community-specific data that can inform programs, policies, and practices to address health disparities and improve the health and well-being of children with ASD.
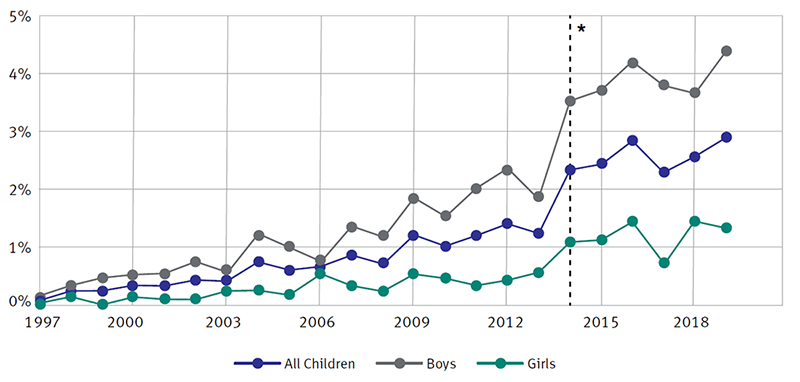
The NHIS is a nationally representative household survey conducted by the National Center for Health Statistics (NCHS). The main objective of the NHIS is to monitor the health of the U.S. population through the collection and analysis of data on a broad range of health topics, including the presence of developmental disorders among children. A major strength of this survey lies in the ability to categorize these health characteristics by many demographic and socioeconomic characteristics.
NHIS data are used widely throughout HHS to monitor trends in illness and disability and to track progress toward achieving national health objectives. The data are also used by the public health research community for epidemiologic and policy analysis of such timely issues as characterizing those with various health problems, determining barriers to accessing and using appropriate health care, and evaluating federal health programs. The NHIS collects data continuously throughout the year with an annual release, thereby allowing for annual prevalence estimates of ASD, intellectual disability, attention-deficit/hyperactivity disorder (ADHD), developmental delay, and learning disability. The NHIS is not named in, nor does it receive authorization under, the Autism CARES Act of 2019 but is instead authorized by Title 42 of the U.S. Code (U.S.C.), Section 242k.
CDC’s Study to Explore Early Development (SEED) is a case-control study of children aged 2-5 years with ASD compared to children with other developmental delays and disabilities and to children from the general population. SEED contributes to knowledge about risk factors for ASD and describes the behavioral phenotypes, co-occurring health conditions, and health care services and needs of children with ASD or with other developmental disabilities. With the release of data from the final phase of SEED, data are now available for over 6,000 children, including over 1,800 children with ASD.
SEED data are being used to:
- Explore risk factors that may be related to the development of ASD.
There are likely many causes of ASD, and there may be many different factors that make a child more likely to have ASD, including environmental, biologic, and genetic factors. SEED data have been used to look at factors associated with ASD, including maternal infections,15 maternal hormonal factors (such as infertility conditions and treatments), maternal psychiatric history and use of selective serotonin reuptake inhibitors,16 maternal weight gain during pregnancy,17 obesity, and air pollution and neighborhood deprivation.18 - Help inform care and treatment decisions for children with ASD.
SEED data also have been used to examine health and behavior characteristics of children with ASD, such as gastrointestinal symptoms,19 wandering,20 pica,21 resistance to toilet training,22 and sleep problems.23 The diverse nature of ASD can make it difficult to find risk factors and treatment options. SEED data were used to identify the most dissimilar and most similar symptom(s) in children classified as ASD and as having subthreshold ASD characteristics.24 - Examine existing services and supports.
SEED data have shown that approximately 60% of children with ASD who use psychotropic medications have not received behavior therapy, despite recommendations from the American Academy of Pediatrics that behavior therapy should be used as a first-line treatment.25 Researchers have used SEED data to examine use of community-based services for preschool-aged children and the importance of having insurance.26 - Assess the impact of COVID-19.
In 2020, CDC leveraged SEED infrastructure to collect information on the impact of COVID-19 on services, behaviors, and health to help inform public health strategies for young children with and without ASD (aged 3-8 years) and their families during public health emergencies. These data have been used to compare children with ASD to children with other developmental disabilities and to children from the general population regarding their experiences with disruptions to regular health care, developmental services, classroom accommodations received through IDEA, and IEP or 504 plan goals. Analyses have been completed for the following topics: changes in daily living skills and behavior problems from before to after the onset of the pandemic; use of telehealth services and parent training for delivering therapies; factors associated with childhood resiliency; response to mitigation strategies and infection; and the impact of COVID on parental mental health. - Identify the health care needs of teens with ASD.
In FY 2021, CDC completed SEED Teen, a follow-up study of original SEED participants at ages 12-16 years, and reported preliminary data indicating adolescents with autism were 90% more likely to have additional mental health or other conditions and three times more likely to have unmet health care service needs compared with children in the general population.27 - Learn more about how people with ASD develop over time from childhood to adolescence and adulthood.
CDC used lessons learned from SEED Teen to inform SEED Follow-Up, launched in summer 2023. Data collected in SEED Follow-Up will facilitate analyses on early adult outcomes of individuals with ASD (e.g., health, functioning, and service use and needs) and factors associated with developmental trajectories. Additional components of SEED Follow-Up are in-person examination of cognitive abilities of individuals with and without ASD and analysis of existing data and biospecimens from preschool-aged participants and their families.
CDC’s Learn the Signs. Act Early. encourages early, ongoing, and family-engaged developmental monitoring of all children and early identification of developmental delays and disabilities so that children and their families can receive the services and support they need. The program provides free tools and resources in English, Spanish, and other languages, such as the Milestone Tracker app, for families and professionals. Between January 2019 through September 2023, there were more than 12.1 million Learn the Signs. Act Early. materials distributed. The Learn the Signs. Act Early. webpages have received more than 42.5 million page views. The Milestone Tracker app has had over 1.8 million downloads and 4.7 million uses (users launching the app). From January 2020 through September 2023, 120,500 people completed the Watch Me! training. These materials, webpages, app, and trainings are utilized by parents, health care professionals, early childcare providers, partners, program champions like Act Early Ambassadors, and other early childhood professionals.
In 2022, CDC made available the revised developmental milestone checklists and other Learn the Signs. Act Early. materials. These revisions are intended to better support ongoing conversations about children’s development between families and professionals. They also help promote early identification of and action on potential developmental concerns so that children and families can get the early services and support they may need.
Learn the Signs. Act Early. has worked to establish partnerships to integrate developmental monitoring into programs and systems that serve young children and their families, including public health programs and childcare programs. There continues to be a particular focus on reaching low-resource families through partnerships with the U.S. Department of Agriculture. Over the past year, technical assistance and collaborative learning opportunities were provided to Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) staff from 22 states and one territory; WIC programs in 19 states are assisting with the dissemination of CDC’s free Milestone Tracker app; and WIC staff from 44 states have participated in training on early development. CDC’s Learn the Signs. Act Early. program also funds the American Academy of Pediatrics through a cooperative agreement to target messaging to pediatric health care providers about the importance of developmental monitoring, screening, referral, and follow-up. The Learn the Signs. Act Early. program develops and promotes training and materials to support health care and other providers’ roles in assuring these services.
CDC has also funded seven cohorts of Act Early Ambassadors since 2011 though cooperative agreements with the Association of University Centers on Disabilities (AUCD). Ambassadors are state, tribal, or territorial leaders working to increase collaboration and coordination among early childhood programs by promoting integration of family-engaged developmental monitoring using Learn the Signs. Act Early. tools to help improve early identification of children with developmental delays and disabilities. As of October 2023, the program has grown to 60 Ambassadors across 49 states and the District of Columbia (two Ambassadors each in California, Florida, Illinois, Louisiana, New York, and Texas), three territories (Guam, Northern Mariana Islands, and Puerto Rico), three tribal communities (Alaska, California, and New Mexico), and one Freely Associated State (Federated States of Micronesia). This program has proven to be very effective in putting developmental monitoring into practice. Act Early Ambassadors continue to succeed in integrating developmental monitoring resources into state or territory-wide early childhood systems, including childcare, home visiting, maternal-child health programs, Help Me Grow, early intervention, and care coordination.
With the addition of Coronavirus Aid, Relief, and Economic Security (CARES) Act funds, CDC bolstered the Learn the Signs. Act Early. program to address challenges to early identification and access to supports for children with autism and other developmental disabilities due to the COVID-19 pandemic. CDC funded the AUCD through a cooperative agreement to complete a rapid needs assessment through 43 Act Early Response Teams to inform strategies to mitigate the impact of the COVID-19 pandemic on early identification of developmental delays within early childhood systems. The Act Early Response Teams helped to identify promising practices to reduce the impact of the pandemic on early identification and service delivery. Strategies included adding Deputy Ambassadors to expand access to early identification materials throughout a state or territory, as well as developing and implementing customized partner work plans to increase parent-engaged developmental monitoring and early action on concerns about children, bolstering early childhood systems and delivery of essential health services.
Understanding ASD and its impact on families has been a focus of the National Centers on Birth Defects and Developmental Disabilities (NCBDDD) at CDC for the past 24 years, and it continues to be a major component of its activities. CDC participates as a statutory member agency on the IACC and is also a member of the FIWA. CDC-funded projects and agency activities address all seven Question areas of the IACC Strategic Plan. NCBDDD science and communication investments such as the ADDM Network, SEED, and Learn the Signs. Act Early. specifically address Question 1 (Screening and Diagnosis), Question 3 (Genetic and Environmental Factors), and Question 7 (Infrastructure and Prevalence); numerous other science and communication products are in progress that will facilitate implementation of these and other IACC Strategic Plan goals.
Listed below are a sample of materials developed or additional information from NCBDDD programs and their relation to the IACC Strategic Plan.
- Question 1: Screening and Diagnosis
- Farmer JE, Falk LW, Clark MJ, Mayfield WA, Green KK. Developmental Monitoring and Referral for Low-Income Children Served by WIC: Program Development and Implementation Outcomes. Matern Child Health J. 2022 Feb;26(2):230-241. [PMID: 34988863]
- Zubler J, Whitaker T. CDC's Revised Developmental Milestone Checklists. Am Fam Physician. 2022 Oct;106(4):370-371. [PMID: 36260888]
- Nestor C, Sonikar P, Eberhardt A, Ajiboye AS, Tinker S, Green KK. Exploring parent-engaged developmental monitoring of young children before and during the COVID-19 pandemic, Porter Novelli Styles 2019 and 2021. Disabil Health J. 2023 Jul;16(3):101474. [PMID: 37150662]
- Free Learn the Signs. Act Early. materials, including
- Milestone Tracker app,
- Watch Me! training,
- Milestone booklets and checklists, and
- Children’s books (e.g., Baby’s Busy Day: Being One Is So Much Fun!).
- Question 2: Biology
- Wiggins LD, Tian LH, Rubenstein E, Schieve L, Daniels J, Pazol K, DiGuiseppi C, Barger B, Moody E, Rosenberg S, Bradley C, Hsu M, Robinson Rosenberg C, Christensen D, Crume T, Pandey J, Levy SE. Features that best define the heterogeneity and homogeneity of autism in preschool-age children: A multisite case-control analysis replicated across two independent samples. Autism Res. 2022 Mar;15(3):539-550. [PMID: 34967132]
- Question 3: Genetic and Environmental Factors
- Ames JL, Ladd-Acosta C, Fallin MD, Qian Y, Schieve LA, DiGuiseppi C, Lee LC, Kasten EP, Zhou G, Pinto-Martin J, Howerton EM, Eaton CL, Croen LA. Maternal Psychiatric Conditions, Treatment With Selective Serotonin Reuptake Inhibitors, and Neurodevelopmental Disorders. Biol Psychiatry. 2021 Aug 15;90(4):253-262. [PMID: 34116791]
- Matias SL, Pearl M, Lyall K, Croen LA, Kral TVE, Fallin D, Lee LC, Bradley CB, Schieve LA, Windham GC. Maternal prepregnancy weight and gestational weight gain in association with autism and developmental disorders in offspring. Obesity (Silver Spring). 2021 Sep;29(9):1554- 1564. [PMID: 34347372]
- McGuinn LA, Windham GC, Messer LC, Di Q, Schwartz J, Croen LA, Moody EJ, Rappold AG, Richardson DB, Neas LM, Gammon MD, Schieve LA, Daniels JL. Air pollution, neighborhood deprivation, and autism spectrum disorder in the Study to Explore Early Development. Environ Epidemiol. 2019 Oct;3(5):e067. [PMID: 32478281]
- Christensen D, Pazol K, Overwyk KJ, England LJ, Alexander AA, Croen LA, Dowling NF, Schieve LA, Tian LH, Tinker SC, Windham GC, Callaghan WM, Shapira SK. Prenatal ultrasound use and risk of autism spectrum disorder: Findings from the case-control Study to Explore Early Development. Paediatr Perinat Epidemiol. 2023 Aug;37(6): 527-535. [PMID: 37483151]
- Question 4: Interventions
- Wiggins LD, Nadler C, Rosenberg S, Moody E, Reyes N, Reynolds A, Alexander A, Daniels J, Thomas K, Giarelli E, Levy SE. Many Young Children with Autism Who Use Psychotropic Medication Do Not Receive Behavior Therapy: A Multisite Case-Control Study. J Pediatr. 2021 May;232:264-271. [PMID: 33493493]
- Question 5: Services and Supports
- Rubenstein E, Croen L, Lee LC, Moody E, Schieve LA, Soke GN, Thomas K, Wiggins L, Daniels J. Community-based service use in preschool children with autism spectrum disorder and associations with insurance status. Res Autism Spectr Disord. 2019 Oct;66:101410. [PMID: 32831903]
- Wiggins LD, Durkin M, Esler A, Lee LC, Zahorodny W, Rice C, Yeargin-Allsopp M, Dowling NF, Hall-Lande J, Morrier MJ, Christensen D, Shenouda J, Baio J. Disparities in Documented Diagnoses of Autism Spectrum Disorder Based on Demographic, Individual, and Service Factors. Autism Res. 2020 Mar;13(3):464-473. [PMID: 31868321]
- Esler AN, Sample J, Hall-Lande J, Harris B, Rice C, Poynter J, Kirby RS, Wiggins L. Patterns of Special Education Eligibility and Age of First Autism Spectrum Disorder (ASD) Identification Among US Children with ASD. J Autism Dev Disord. 2023 May;53(5):1739-1754. [PMID: 35212866]
- Furnier SM, Ellis Weismer S, Rubenstein E, Gangnon R, Rosenberg S, Nadler C, Wiggins LD, Durkin MS. Using adaptive behavior scores to convey level of functioning in children with autism spectrum disorder: Evidence from the Study to Explore Early Development. Autism. 2023 Aug 23:13623613231193194. [PMID: 37609907]
- Question 6: Lifespan
- Powell PS, Pazol K, Wiggins LD, Daniels JL, Dichter GS, Bradley CB, Pretzel R, Kloetzer J, McKenzie C, Scott A, Robinson B, Sims AS, Kasten EP, Fallin MD, Levy SE, Dietz PM, Cogswell ME. Health Status and Health Care Use Among Adolescents Identified With and Without Autism in Early Childhood - Four U.S. Sites, 2018-2020. MMWR Morb Mortal Wkly Rep. 2021 Apr 30;70(17):605- 611. [PMID: 33914722]
- Hughes MM, Shaw KA, Patrick ME, DiRienzo M, Bakian AV, Bilder DA, Durkin MS, Hudson A, Spivey MH, DaWalt LS, Salinas A, Schwenk YD, Lopez M, Baroud TM, Maenner MJ. Adolescents With Autism Spectrum Disorder: Diagnostic Patterns, Co-occurring Conditions, and Transition Planning. J Adolesc Health. 2023 Aug;73(2):271- 278. [PMID: 36849336]
- Hughes MM, Kirby AV, Davis J, Bilder DA, Patrick M, Lopez M, DaWalt LS, Pas ET, Bakian AV, Shaw KA, DiRienzo M, Hudson A, Schwenk YD, Baroud TM, Washington A, Maenner MJ. Individualized Education Programs and Transition Planning for Adolescents With Autism. Pediatrics. 2023 Jul 1;152(1):e2022060199. [PMID: 37345494]
- CDC aims to increase inclusion of people with disabilities, including ASD, in public health data to better evaluate health disparities, target disease prevention and health promotion activities, and evaluate health and other outcomes. These efforts include increased collaborations to include the HHS Disability Data Standard in public health data collection systems and to enhance the use of administrative and survey data in identifying people with disabilities.
- CDC funds two National Programs on Health Promotion for People with Disabilities — the National Center on Health, Physical Activity, and Disability and Special Olympics — to work with people with mobility limitations and intellectual disabilities, respectively. These national organizations support the development, implementation, evaluation, and dissemination of non-research activities aimed at raising knowledge and awareness of the health needs of people with mobility limitations and/or intellectual disabilities; developing and disseminating health promotion models, strategies, tools, and health promotion materials; providing training and education to health care professionals; and promoting the adoption of healthy behaviors aimed at reducing health disparities for people with mobility limitations and intellectual disabilities. CDC’s Disability and Health Branch has funded the Special Olympics Healthy Athletes (since 2002) and Healthy Communities (starting in 2012) programs through cooperative agreements to provide Special Olympics athletes with increased access to free health screenings, education, and referrals for follow-up health care, as well as year-round health promotion and disease prevention programs.
- CDC currently funds 10 State Disability and Health Programs through cooperative agreements to improve health outcomes among people with mobility limitations and intellectual disabilities. The state programs strengthen partnerships and design, create, and implement programs to improve the health of people with disabilities in their states. In 2021, CDC began a new five-year cycle with an increased focus on expanding and enhancing jurisdictional and statewide partnerships; administering and evaluating training on accessible preventive health care among health care providers; linking people with intellectual and developmental disabilities to preventative health care and health promotion programs; and implementing evidence-based interventions and policy, system, and environmental changes.
- Additionally, in 2020, CDC partnered with the Association of State and Territorial Health Officials and the National Association of County and City Health Officials (NACCHO) through a cooperative agreement to embed 28 disability specialists within state, territorial, and local health departments to help ensure issues impacting people with disabilities are considered in planning and response efforts. Specialists completed baseline needs assessments and worked with their assigned jurisdiction to update emergency response plans to better serve the needs of people with disabilities. In 2022, CDC supported a second cohort of the NACCHO Disability Specialists Program through a separate cooperative agreement to embed 11 additional disability specialists within local health departments.
- Question 7: Infrastructure and Prevalence
- Maenner MJ, Graves SJ, Peacock G, Honein MA, Boyle CA, Dietz PM. Comparison of 2 Case Definitions for Ascertaining the Prevalence of Autism Spectrum Disorder Among 8-Year-Old Children. Am J Epidemiol. 2021 Oct 1;190(10): 2198-2207. [PMID: 33847734]
- Shaw KA, McArthur D, Hughes MM, Bakian AV, Lee LC, Pettygrove S, Maenner MJ. Progress and Disparities in Early Identification of Autism Spectrum Disorder: Autism and Developmental Disabilities Monitoring Network, 2002-2016. J Am Acad Child Adolesc Psychiatry. 2022 Jul;61(7):905-914. [PMID: 34838692]
- Shaw KA, Williams S, Hughes MM, Warren Z, Bakian AV, Durkin MS, Esler A, Hall-Lande J, Salinas A, Vehorn A, Andrews JG, Baroud T, Bilder DA, Dimian A, Galindo M, Hudson A, Hallas L, Lopez M, Pokoski O, Pettygrove S, Rossow K, Shenouda J, Schwenk YD, Zahorodny W, Washington A, Maenner MJ. Statewide county-level autism spectrum disorder prevalence estimates-seven U.S. states, 2018. Ann Epidemiol. 2023 Mar; 79:39-43. [PMID: 36669598]
- Etyemez S, Esler A, Kini A, Tsai PC, DiRienzo M, Maenner M, Lee LC. The role of intellectual disability with autism spectrum disorder and the documented cooccurring conditions: A population-based study. Autism Res. 2022 Dec;15(12):2399-2408. [PMID: 36245337]
- Hughes MM, Shaw KA, DiRienzo M, Durkin MS, Esler A, Hall-Lande J, Wiggins L, Zahorodny W, Singer A, Maenner MJ. The Prevalence and Characteristics of Children With Profound Autism, 15 Sites, United States, 2000-2016. Public Health Rep. 2023 Apr 19:333549231163551. [PMID: 37074176]
- Shaw KA, Bilder DA, McArthur D, Williams AR, Amoakohene E, Bakian AV, Durkin MS, Fitzgerald RT, Furnier SM, Hughes MM, Pas ET, Salinas A, Warren Z, Williams S, Esler A, Grzybowski A, Ladd-Acosta CM, Patrick M, Zahorodny W, Green KK, Hall-Lande J, Lopez M, Mancilla KC, Nguyen RHN, Pierce K, Schwenk YD, Shenouda J, Sidwell K, Vehorn A, DiRienzo M, Gutierrez J, Hallas L, Hudson A, Spivey MH, Pettygrove S, Washington A, Maenner MJ. Early Identification of Autism Spectrum Disorder Among Children Aged 4 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2020. MMWR Surveill Summ. 2023 Mar 24;72 (1):1-15. [PMID: 36952289]
- Maenner MJ, Warren Z, Williams AR, Amoakohene E, Bakian AV, Bilder DA, Durkin MS, Fitzgerald RT, Furnier SM, Hughes MM, Ladd-Acosta CM, McArthur D, Pas ET, Salinas A, Vehorn A, Williams S, Esler A, Grzybowski A, Hall-Lande J, Nguyen RHN, Pierce K, Zahorodny W, Hudson A, Hallas L, Mancilla KC, Patrick M, Shenouda J, Sidwell K, DiRienzo M, Gutierrez J, Spivey MH, Lopez M, Pettygrove S, Schwenk YD, Washington A, Shaw KA. Prevalence and Characteristics of Autism Spectrum Disorder Among Children Aged 8 Years - Autism and Developmental Disabilities Monitoring Network, 11 Sites, United States, 2020. MMWR Surveill Summ. 2023 Mar 24;72 (2):1-14. [PMID: 36952288]
- Zablotsky B, Ng AE, Black LI, Blumberg SJ. Diagnosed Developmental Disabilities in Children Aged 3-17 Years: United States, 2019-2021. NCHS Data Brief. 2023 Jul;(473): 1-8. [PMID: 37440277]
Table 5: CDC ASD-Related Expenditures, FY 2019 – FY 2023.
| CDC ASD-Related Expenditures: FY 2019 – FY 2023 | |
|---|---|
| Fiscal Year | Autism Surveillance and Research* and Awareness of Developmental Milestones and Early Identification (Learn The Signs. Act Early.)** |
Fiscal Year2019 |
Autism Surveillance And Research$18,720,000 |
Fiscal Year2020 |
Autism Surveillance And Research$18,517,154 |
Fiscal Year2021 |
Autism Surveillance And Research$18,460,799 |
Fiscal Year2022 |
Autism Surveillance And Research$18,645,561 |
Fiscal Year2023 |
Autism Surveillance And Research$23,411,640 |
Fiscal YearTotal |
Autism Surveillance And Research$97,755,154 |
* Autism Surveillance and Research is authorized under the Autism CARES Act of 2019. These expenditures include costs associated with CDC’s autism budget lines in support of programs on autism and other developmental disabilities. Appropriations for these activities are a part of the annual appropriations provided to CDC and are not appropriated under the Autism CARES Act of 2019.
** Awareness of Developmental Milestones and Early Identification (Learn the Signs. Act Early.) is authorized under the Autism CARES Act of 2019. These expenditures include costs associated with CDC’s autism budget lines in support of programs on autism and other developmental disabilities. Appropriations for these activities are a part of the annual appropriations provided to CDC and are not appropriated under the Autism CARES Act of 2019.
Centers for Medicare & Medicaid Services (CMS)
The Centers for Medicare & Medicaid Services (CMS) is committed to strengthening and modernizing the nation’s health care system to enhance quality, accessibility, and improved outcomes in the most cost-effective manner possible. CMS administers several programs that are available to individuals with disabilities, including those with ASD. These programs do not receive appropriations from the Autism CARES Act of 2019.
The Medicaid program is a state-federal partnership, funded jointly by states and the federal government, which provides health coverage to millions of Americans, including eligible low-income adults, children, pregnant people, elderly adults, and people with disabilities. States establish and administer their own Medicaid programs and determine the type, amount, duration, and scope of services within broad federal guidelines. Federal law requires states to provide certain mandatory benefits and allows states the choice of covering other optional benefits; therefore, there is variation across states in terms of the scope of coverage offered in each Medicaid program. Individuals with ASD could receive some of these mandatory and optional services based on their individually assessed needs. Examples of mandatory benefits include inpatient and outpatient hospital services, physician services, laboratory and x-ray services, and home health services, among others. Optional benefits include prescription drug coverage, case management, physical therapy, occupational therapy, and HCBS. HCBS provide opportunities for Medicaid beneficiaries, including individuals on the autism spectrum, to receive services in their own home or community rather than institutional settings. Detailed information on HCBS provided through Medicaid programs are described on page 125.
For states with managed care plans, those plans are expected to offer the services they are contracted with the state to provide, including those specific to ASD, without adding unnecessary barriers to service access. Federal law requires that state Medicaid programs, including Medicaid managed care plans, ensure adequate access to timely care, including by keeping an adequate network of providers. Individuals eligible for Medicaid via the adult group receive a benefit package that includes essential health benefits (EHBs; see next paragraph), including hospitalization, preventive services, and prescription drugs, to help ensure that individuals have the coverage needed to stay healthy.
Services and supports for individuals with ASD can be covered under Medicaid through a variety of authorities, including under mandatory and optional benefits described in Section 1905(a) of the Social Security Act. CMS does not endorse or require any particular treatment modality for ASD. State Medicaid agencies are responsible for determining what services are included within a menu of both mandatory and optional services for eligible individuals. Medicaid may cover a variety of services and supports, such as case management; rehabilitative services; physical, occupational; and speech therapies. The following benefit categories are the most common benefits that states use to provide services to address ASD: Section 1905(a)(6), Services of Other Licensed Practitioners; Section 1905(a)(13), Preventive Services; and Section 1905(a)(11), Therapies. Additionally, Section 1937 of the Social Security Act requires that EHBs be provided to beneficiaries enrolled in alternative benefit plans (benchmark or benchmark-equivalent coverage). EHBs include coverage of a broad range of services including habilitative services, which are central to care and treatment for people with ASD.
Section 1905(r) of the Social Security Act specifies requirements related to the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) benefit, a mandatory benefit extended to all Medicaid-eligible individuals under the age of 21. Medicaid’s EPSDT benefit requires the provision of any medically necessary health care services listed in Section 1905(a) and includes a comprehensive array of preventive, diagnostic, and treatment services, as well as services to address ASD, for low-income infants, children, and adolescents under age 21. The EPSDT benefit requires screening services as well as physical, mental, vision, hearing, and dental services for such persons under age 21 that are needed to correct or ameliorate health conditions, based on certain federal guidelines.
The Children’s Health Insurance Program (CHIP) provides comprehensive health coverage to uninsured children in families with incomes too high to qualify for Medicaid but too low to afford private coverage. States have the flexibility to design their own CHIP within federal guidelines and may choose between a funded Medicaid expansion program, a separate CHIP, or a combination of both types of programs. States that establish and administer their own separate CHIPs determine the type, amount, duration, and scope of services within broad federal guidelines. Federal law requires states to provide certain mandatory benefits and allows states the choice of covering other optional benefits; therefore, there is variation across states in terms of the scope of coverage offered in each separate CHIP program. For example, some states specifically include coverage of applied behavior analysis (ABA) as part of their CHIP benefits available for the screening, diagnosis, and treatment of individuals with ASD. All separate CHIPs must provide well-baby and well-child health care, dental coverage, behavioral health care, and vaccines. Section 2103(c)(5) of the Social Security Act requires coverage of mental health services, including behavioral health treatment, necessary to prevent, diagnose, and treat a broad range of mental health symptoms and disorders. CHIP beneficiaries in states providing Medicaid-expansion receive the EPSDT benefits described above. Child beneficiaries in states providing a separate CHIP receive a set of benefits that may (but are not required to) include the EPSDT benefit. Approximately 15 states have elected to cover the EPSDT benefit in their separate CHIPs.
In August 2022, CMS announced key actions to strengthen and expand access to high-quality, comprehensive health care for children, including children with autism, across the country. CMS issued new guidance reminding states of their mandate to cover behavioral health services under the EPSDT benefit and separate guidance urging states to leverage every resource to strengthen mental health care for children, including through the expansion of school-based health care. HHS also issued a proposed rule that would make it mandatory for states to report certain quality measures for the first time ever to strengthen Medicaid and CHIP and to ensure that the millions of children and families enrolled in these programs have access to the highest quality of care. These actions are part of HHS’s ongoing efforts to support the Biden-Harris Administration’s call to address the nation’s mental health crisis, including its impact on children.
CMS released guidance in April 2023 to encourage states to apply for a new demonstration project opportunity under Section 1115(a) of the Social Security Act (commonly referred to as the Medicaid Reentry Section 1115 Demonstration opportunity) to help increase care for individuals who are incarcerated, including those with autism, in the period immediately prior to their release to help them succeed and thrive as they reenter their communities. The new demonstration opportunity would allow state Medicaid programs to cover services that address various health concerns, including substance use disorders and other chronic health conditions.
In April 2023, CMS published two notices of proposed rulemaking, Ensuring Access to Medicaid Services and Managed Care Access, Finance, and Quality, that together, if finalized, would further strengthen access to and quality of care across Medicaid and CHIP. If adopted as proposed, the rules would establish historic national standards for access to care regardless of whether that care is provided through managed care plans or directly by states through fee-for-service. Specifically, they would establish access standards through Medicaid or CHIP managed care plans, as well as transparency for Medicaid payment rates to providers, including hourly rates and compensation for certain home care and other direct care workers, including those who support individuals with autism. The rules would also establish other access standards for transparency and accountability and empower beneficiary choice, such as through creating new quality reporting and quality improvement requirements and standardizing and strengthening incident management system and person-centered planning requirements for HCBS programs.
While CMS does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by CMS are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. CMS activities are also relevant to Question 5 (Services and Supports) and Question 6 (Lifespan) of the IACC Strategic Plan. CMS is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Food and Drug Administration (FDA)
The mission of the Food and Drug Administration (FDA) is to protect and advance public health by ensuring food safety and by helping to speed innovations that provide the nation with safe and effective medical products. The FDA achieves this by applying the latest technology and science-based standards to the regulatory challenges presented by drugs, biologics (i.e., vaccines, blood products, cell and gene therapy products, and tissues), medical devices, food additives, and, since 2009, tobacco. The FDA reviews protocols for clinical trials to assess study design and ensure the protection of human subjects. The FDA also reviews new drug applications to ensure that new drugs are safe and effective. Drugs used to ameliorate various symptoms of autism including anxiety, depression, aggression, and seizures are a few of the many pharmacologic treatments that are subject to rigorous regulatory review by the FDA.
The FDA’s Center for Drug Evaluation and Research (CDER) regulates over-the-counter and prescription drugs, including biological therapeutics and generic drugs, and ensures that safe and effective drugs are available to improve the health of people in the United States. The mission of the CDER Biomarker Qualification Program (BQP), funded by the 21st Century Cures Act and the Prescription Drug User Fee Act, is to work with external stakeholders to develop biomarkers as drug development tools. Qualified biomarkers have the potential to advance public health by encouraging efficiencies and innovations in drug development. The goals of the program are to support outreach to stakeholders for the identification and development of new biomarkers, provide a framework for the review of biomarkers for use in regulatory decision-making, and qualify biomarkers for specific contexts of use that address specified drug development needs.
The BQP has supported two autism biomarker projects and reviewed three regulatory submissions for these projects. These projects were submitted by the Autism Biomarkers Consortium for Clinical Trials (ABC-CT), an NIH-funded multicenter research study based at Yale University and spans Duke University, Boston Children’s Hospital, the University of Washington/Seattle Children’s Research Institute, and the University of California, Los Angeles. In addition, these projects have qualified and received two grants from the FDA to develop these projects from the 21st Century Cures Act (1U01FD006888-01 and 1U01FD007000-01). Each grant was $250,000. The goal of these projects is to develop biomarkers to identify a subset of ASD patients with specific characteristics based on putative biomarkers such as the N170 signal to upright faces and the oculomotor index of orienting to human faces. Patients with similar findings on these measures may share similar underlying biology, which may help to identify targets for drug development.
The FDA’s Center for Devices and Radiological Health (CDRH) facilitates medical device innovation by advancing regulatory science, providing industry with predictable, consistent, transparent, and efficient regulatory pathways, and assuring consumer confidence in devices marketed in the United States. In 2021, the FDA authorized marketing of the Cognoa ASD Diagnosis Aid to help diagnose ASD in children 18 months through 5 years of age. The device uses machine learning algorithm and consists of a mobile app for caregivers and parents to answer questions about their children’s behavior and to upload videos of their child; a video analysis portal that allows manufacturer-trained and certified specialists to view and analyze uploaded videos of patients; and a health care provider portal that is intended for a health care provider to enter answers to pre-loaded questions about child behaviors, track the information provided by parents and caregivers, and review a report of the results. The ASD Diagnosis Aid processes the information provided by parents, caregivers, and health care providers and reports a positive or negative diagnosis if there is sufficient information for its algorithm to make a determination. The FDA reviewed the Cognoa ASD Diagnosis Aid through the De Novo premarket review pathway, a regulatory pathway for low- to moderate-risk devices of a new type. The device is not indicated for use as a stand-alone diagnostic device but as an adjunct to the diagnostic process.
In July 2023, EarliTec Diagnostics, Inc., received FDA 510(k) authorization of its second generation EarliPoint Evaluation for ASD for children ages 16 to 30 months old. The EarliPoint Evaluation displays scenes of social interaction on a portable tablet and uses eye-tracking technology to measure a child’s Social-Visual Engagement. The data is reviewed and compared to age-expected reference metrics to determine if the child is missing key moments of social learning. A personalized and detailed report is created for clinician review to determine the presence of autism, the severity of social disability, and level of verbal ability and non-verbal learning.
While the FDA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, FDA activities impact individuals with ASD and their families. These activities are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. Research funded by the FDA additionally address Question 1 (Screening and Diagnosis), Question 2 (Biology), and Question 4 (Interventions) of the IACC Strategic Plan. The FDA is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Health Resources and Services Administration (HRSA)
The Health Resources and Services Administration (HRSA) is dedicated to providing equitable health care to the nation’s highest need communities. HRSA serves people who are geographically isolated and economically or medically vulnerable. Under the Autism CARES Act of 2019, HRSA received funding to increase awareness of ASD and other developmental disabilities; reduce barriers to screening and diagnosis; support research on evidence-based interventions; promote the development of guidelines for evidence-based practices; and train health care professionals to provide screening, diagnostic, and evidence-based early intervention services for children with a confirmed diagnosis. To meet these objectives, HRSA funded grant programs in three areas: Training, Research, and State Systems Development. HRSA also funded two national resource centers to provide technical assistance to and promote collaboration among grantees.
Through their collective efforts, HRSA’s programs improve care and outcomes for children, adolescents, and young adults with autism and other developmental disabilities. A description of significant progress follows.
HRSA supports 60 Leadership Education in Neurodevelopmental and Other Related Disabilities (LEND) Training programs and 13 Developmental- Behavioral Pediatrics (DBP) Training programs to address the shortage of trained professionals who can provide screening, diagnostic services, and treatment for individuals with autism and other developmental disabilities. Programs are in 45 states, with partnerships that extend to the five remaining states and several U.S. jurisdictions. In 2021, HRSA expanded the LEND program from 52 to 60 awards. In 2023, HRSA expanded the DBP program from 12 to 13 awards.
Interdisciplinary clinics associated with the LEND and DBP training programs are making evidence-based interdisciplinary services available across the nation, particularly in communities that are historically underserved. The LEND programs provide interdisciplinary clinical training and leadership development to professionals from multiple disciplines who have a role in identifying, evaluating, or caring for children with autism and other developmental disabilities. The DBP training programs prepare developmental-behavioral pediatric fellows with essential biopsychosocial knowledge and expertise and for leadership roles as teachers, investigators, and clinicians. Each year, the LEND and DBP programs enroll long-term fellows to receive at least 300 hours of intensive didactic training and clinical experience working in hospitals, clinics, and community-based settings that provide diagnostic or intervention services for individuals with autism and other developmental disabilities. Collectively, the programs also provide graduate level training to other health professionals, including medical residents, to increase their understanding of autism and other developmental disabilities and make them aware of emerging evidence regarding autism evaluation and services, and to family members and self-advocates.
From FY 2018 – FY 2021, the LEND and DBP programs collectively reached more than 6,400 long-term trainees, 18,000 medium-term trainees, and 62,000 short-term trainees. Long-term trainees are those who received 300 or more hours of training, medium-term trainees receive 40 to 299 hours of training, and short-term trainees receive less than 40 hours of training through the HRSA-funded training programs. By preparing these professionals to implement recommended screening practices and use evidence-based diagnostic tools, the training programs are improving early identification of autism and other developmental disabilities. The training programs also reach an extensive network of providers with continuing education, with over 1.1 million participants from FY 2018 – FY 2021.
Data collected from the LEND and DBP programs show the direct impact of these investments on individuals with autism and their families. From FY 2018 – FY 2021, the programs provided interdisciplinary diagnostic services for more than 492,000 individuals. By continuing to meet the growing demand for services, the programs are reducing wait times for diagnostic evaluation and entry into intervention services. The training programs are helping to address disparities in early identification of autism by expanding their reach to underserved populations through innovative mechanisms, including telehealth and tele-consultation.
HRSA’s autism research programs currently support four national autism Research Networks, two Autism Single Investigator Innovation Programs (Autism SIIP), the Autism Field-Initiated Research Studies (Autism FIRST) program, and the Autism Secondary Data Analysis Research (Autism SDAR) program to advance the evidence base on effective interventions to improve the health and well-being of children and adolescents with autism and other developmental disabilities. These programs address the needs of people who are underserved, such as people with lower incomes, people from racial/ethnic minority groups, and individuals who have limited access to services. In FY 2021, the autism research programs collectively enrolled over 17,000 participants in primary studies and over one million participants in secondary studies in 97 studies at 50 sites. Over 350 researchers were engaged in autism research and 69 manuscripts were published in peer-reviewed journals. Tables 29-42 in Appendix IV contain descriptions of the projects/studies and tools/guidelines developed under each autism research program.
The AIR Networks establish and maintain an interdisciplinary, multicenter research forum for scientific collaboration and infrastructure building. They provide national leadership in research to advance the evidence base on effective interventions for children and adolescents with autism and developmental disabilities as they transition to adulthood and across the lifespan. The Research Networks develop guidelines for those interventions and disseminate information related to such research and guidelines, as authorized by the Autism CARES Act of 2019.
- The Autism Intervention Research Network on Physical Health (AIR-P) provides national leadership in research to advance the evidence base on effective interventions for children and adolescents with autism and other developmental disabilities, with a focus on addressing physical health and well-being across the lifespan. Physical health may include, but is not limited to, medical, dental, visual, nutrition, and speech/hearing components.
- The Autism Intervention Research Network on Behavioral Health (AIR-B) provides national leadership in research to advance the evidence base on effective interventions for children and adolescents with autism and other developmental disabilities, with a focus on addressing behavioral health and well-being across the lifespan.
- The Developmental Behavioral Pediatrics Research Network (DBPNet) provides national leadership in research to advance the evidence base in the developmental, behavioral, and psychosocial aspects of pediatric care. DBPNet works to develop effective interventions in clinical services and health and related outcomes for children and adolescents with autism and other developmental disabilities across the lifespan.
- The Healthy Weight Research Network (HWRN) for Children with ASD and Developmental Disabilities provides national leadership in research designed to improve the promotion of healthy weight through the prevention and treatment of overweight, obesity, and underweight among children and adolescents with autism and other developmental disabilities.
The Autism SIIP program supports two projects focused on priority or emerging autism and developmental disabilities research areas and research topics with limited research.
The Autism Longitudinal Data Project (ALDP) supports the implementation and completion of research studies that examine longitudinal data on autism and other developmental disabilities to study risk factors for these conditions, the effects of various interventions, and trajectories of child development over the life course.
The Autism Transitions Research Project (ATRP) supports the implementation and completion of research studies that examine factors associated with healthy life transitions among adolescents and young adults with autism who are transitioning to adulthood.
The Autism FIRST program supports research studies testing the implementation of new and innovative strategies that address critical issues surrounding the health of children and adolescents with ASD. These is a special focus on addressing the needs of underserved populations and on promoting health and well-being through supports and services offered to children and youth with autism and other developmental disabilities (and their families) up to the age of 21, recognizing that these years lay the foundation for health and well-being across the lifespan.
The Autism SDAR program supports secondary data analyses of national datasets and/or administrative records to advance the evidence base on interventions designed to improve the health and well-being of children and adolescents with autism and other developmental disabilities, with a particular focus on addressing barriers to identification, diagnosis, interventions, and services among underserved populations.
In FY 2019, HRSA funded five grants through the Innovations in Care Coordination for Children and Youth with Autism Spectrum Disorders and Other Developmental Disabilities program. The purpose of the program is to improve access to coordinated and integrated care for children with, or at risk for, autism and other developmental disabilities and their families in medically underserved areas and populations.
In FY 2020, the Innovations in Care grantees partnered with 46 primary care providers to serve 1,074 families through family navigation. Family navigation services included supporting families of children with or at risk for autism and developmental disabilities through resource-sharing, referral information, emotional support, and coaching. In addition to family navigation, the Innovations in Care grantees contributed to increased awareness of autism and other developmental disability topics among providers and the public by providing educational opportunities for health care professionals. Collectively, the grantees held more than 34 webinars for primary care physicians, reaching more than 563 attendees. In addition, grantees provided six parent and community trainings, hosted through their respective learning communities, reaching over 600 participants.
Data provided by state grantees indicate measurable improvements in screening and referral practices. State grantee activities included forming quality improvement learning collaboratives with pediatric practices to increase screening rates and working with communities to strengthen infrastructure and increase the number of professionals using reliable, valid tools to identify children with autism. The Innovations in Care Coordination grantees are the Rectors & Visitors of the University of Virginia, University of Iowa, University of Wisconsin System, Vanderbilt University Medical Center, and University of North Carolina at Chapel Hill.
HRSA supports two additional investments through the Title V Maternal and Child Health (MCH) Services Block Grant program (Section 501(a) of Title V of the Social Security Act). This program intends "to improve the health of all mothers and children consistent with the applicable health status goals and national health objectives." Administered through well-established federal/state partnerships, states have broad discretion in implementing programs that meet their specific priority needs. The grantees are public health programs that are responsible for assessing needs in their state for the entire MCH population and prioritize programs to meet those needs. States and jurisdictions use their Title V funds to design and implement a wide range of activities for MCH and children with special health care needs, which may include children with autism.
The NSCH, funded and directed by HRSA, provides national and state level estimates of key measures of health and well-being of American children 0-17 years old. Information is collected annually on factors including access to and utilization of health care, receipt of care in a medical home, family interactions, parental health, school and after-school experiences, and neighborhood characteristics. The NSCH includes questions on the prevalence of autism, as well as age at diagnosis, type of provider who gave the diagnosis, parent assessment of condition severity, and types of autism treatment received. The NSCH is supported through the Special Projects of Regional and National Significance of the Title V MCH Services Block Grant program (Section 501(a) of Title V of the Social Security Act).
FY 2019 through FY 2023 funding information for the NSCH, as well as total funding for the Title V MCH Services Block Grant program, is listed in Table 6.
Table 6: Funding for HRSA’s Title V MCH Services Block Grant and NSCH, authorized under Section 501(a) of Title V of the Social Security Act.
| Title V MCH Services Block Grant and NSCH Funding: FY 2019 – FY 2023 | ||
|---|---|---|
| Fiscal Year | Title V Services Block Grant | NSCH |
Fiscal Year2019 |
Title V Services Block Grant$543,419,420 |
NSCH$4,400,000 |
Fiscal Year2020 |
Title V Services Block Grant$545,924,488 |
NSCH$4,400,000 |
Fiscal Year2021 |
Title V Services Block Grant$547,380,809 |
NSCH$4,400,000 |
Fiscal Year2022 |
Title V Services Block Grant$554,062,167 |
NSCH$5,400,000 |
Fiscal Year2023 |
Title V Services Block GrantN/A |
NSCH$7,050,000 |
FY 2023 funding data for Title V MCH Services Block Grant was not available at the time this report was written.
HRSA is a statutory member of the IACC and participates as a member agency on the FIWA. In addition, HRSA utilizes the IACC Strategic Plan to inform the development of its research funding opportunities, promoting the support of autism research investments that address priorities of the IACC Strategic Plan, as well as the Autism CARES Act of 2019 and HRSA’s mission. HRSA Research and Training programs together address all seven Question areas of the IACC Strategic Plan.
Table 7: Total Autism CARES Act of 2019 funding for HRSA autism programs.
| Total HRSA Autism Programs Funding: FY 2019 – FY 2023 (thousands of dollars) | |
|---|---|
| Fiscal Year | Total Funding |
Fiscal Year2019 |
Total Funding$50,377 |
Fiscal Year2020 |
Total Funding$52,344 |
Fiscal Year2021 |
Total Funding$53,344 |
Fiscal Year2022 |
Total Funding$54,344 |
Fiscal Year2023 |
Total Funding$56,344 |
Indian Health Service (IHS)
The Indian Health Service (IHS) is the federal agency responsible for providing federal health services to American Indians and Alaska Natives. The provision of health services to members of federally recognized tribes grew out of the special government-to-government relationship between the federal government and Indian tribes. This relationship, established in 1787, is based on Article I, Section 8, of the Constitution, and has been given form and substance by numerous treaties, laws, Supreme Court decisions, and Executive Orders. The IHS is the principal federal health care provider and health advocate for Indian people, and its goal is to raise their health status to the highest possible level. The IHS provides a comprehensive health service delivery system for approximately 2.6 million American Indians and Alaska Natives who belong to 574 federally recognized tribes.
The IHS does not have any programs or funding specifically focused on provisions of the Autism CARES Act of 2019 nor for individuals on the autism spectrum. However, as a federal health care organization, IHS does provide services to American Indian and Alaska Native patients with ASD. As part of the IHS mission to raise the physical, mental, social, and spiritual health of American Indians and Alaska Natives to the highest level, IHS is committed to providing education, training, consultation, and resources to health care providers treating patients with ASD through the IHS Indian Children’s Program (ICP). The IHS Telebehavioral Health Center of Excellence (TBHCE) oversees this national program. The TBHCE equips health care providers working in the IHS, tribal, and urban Indian health system with the training and education needed to provide excellent care for American Indian and Alaska Native youth with ASD and other neurodevelopmental disorders. Trainings have covered a variety of topics, including supporting safety for families of children with neurodevelopmental disorders during COVID-19, ASD and co-occurring disorders, and mindfulness and dance movement therapies for children with ASD. These services are free and open to the public and include no-cost continuing education credits. From FY 2019 – FY 2023, ICP provided 27 webinars on ASD and autism-related topics with a total of 1,360 participants.
To complement these training opportunities and to further support providers, the ICP also offers a provider-to-provider consultation clinic that addresses ASD, fetal alcohol spectrum disorders (FASDs), and other neurodevelopmental issues experienced by American Indian and Alaska Native youth.
While IHS does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by IHS are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. IHS activities are also relevant to Question 4 (Interventions) and Question 5 (Services and Supports) of the IACC Strategic Plan. IHS is a member of the IACC and the FIWA and participates in efforts to coordinate autism activities across the federal government.
Table 8: IHS funding for ASD-related activities, FY 2019 – FY 2022.
| IHS Funding for ASD-Related Activities: FY 2019 – FY 2022 | |
|---|---|
| Fiscal Year | ASD-Focused Spending |
Fiscal Year2019 |
ASD-Focused Spending$11,000 |
Fiscal Year2020 |
ASD-Focused Spending$16,500 |
Fiscal Year2021 |
ASD-Focused Spending$44,000 |
Fiscal Year2022 |
ASD-Focused Spending$55,000 |
The amounts shown in the table do not account for direct health services for the treatment and management of autism. Data for FY 2023 was not available at the time this report was written.
National Institutes of Health (NIH)
The National Institutes of Health (NIH) is the nation’s medical research agency and works to turn scientific discoveries into better health for all. As part of its mission, NIH supports scientific research to better understand the causes and mechanisms underlying ASD, improve methods of early identification and diagnosis, and develop interventions to improve overall health among children, adolescents, and adults with ASD. NIH makes coordinated efforts to invest in a wide range of ASD research, including basic, translational, clinical, and services research.
NIH created the Autism Centers of Excellence (ACE) program in 2007 with a series of five-year awards to launch an intense and coordinated research program to understand the causes of and develop interventions for ASD. The ACE program also seeks to facilitate innovative and cost-effective services for people with ASD throughout the lifespan. The ACEs aim to develop and mentor the next generation of investigators and clinicians in the field of autism research and treatment. The ACE program is supported by NICHD, National Institute on Deafness and Other Communication Disorders (NIDCD), National Institute of Environmental Health Sciences (NIEHS), NIMH, and National Institute of Neurological Disorders and Stroke (NINDS). In September 2022, NIH announced the latest round of support for 10 ACE grants.
The NICHD-supported Eunice Kennedy Shriver Intellectual & Developmental Disabilities Research Centers are located at 15 universities and academic children's hospitals across the United States to provide support for research in intellectual and developmental disabilities, including ASD, and to advance the development of therapeutics and interventions for intellectual and developmental disabilities. Research projects include use of molecular, cellular, and preclinical models to increase understanding of biological mechanisms; technologies to improve assessment, endpoints, and treatments; and interventions and management of co-occurring conditions, including mental health conditions. A shared project across the centers is promoting understanding of rare genomic variants that underlie intellectual and developmental disabilities.
Supported by NIMH, NINDS, NICHD, the National Institute on Aging (NIA), the National Institute on Drug Abuse (NIDA), and the NIH Blueprint, the NIH NeuroBioBank is a network of brain and tissue banks which aims to collect, store, and distribute post-mortem brain and other tissues for research to improve understanding, care, and treatment of individuals with developmental, neurological, and movement disorders. Each of the six sites collects approximately 100 brains per year. NIH coordinates the sharing of post-mortem brain tissues with the neuroscience community.
NIH supports research to identify ASD at the earliest age possible to enable early intervention and improve long-term outcomes.
- NICHD, NIDCD, NIMH, and NINDS are supporting seven studies through the NIH Early Autism Screening Initiative that aim to translate findings related to early signs of ASD into screening tools that can be implemented in community settings (R01MH121363, R01MH121364, R01MH121329, R01MH121345, R01MH121344, R21HD102078, R21HD100372).
- NIMH-supported researchers are focusing on the development and validation of tele-assessment tools for clinic and in-home use to detect ASD in toddlers and preschool-aged children (R21MH118539, R01MH127228, R21MH128790).
NIH supports research to develop, test, and implement high-quality, evidence-based services and supports that maximize quality of life and health for all people with ASD and their families.
- NIMH-supported researchers are examining the impact of universal screening on child behavioral and functional outcomes (R01MH115715). The researchers posit that screening leads to ASD diagnosis at an earlier age and then to earlier ASD-specific interventions, which improve long-term outcomes. The researchers plan to follow 8,000 toddlers in this study, which is the first randomized control trial screening toddlers for ASD and measuring outcomes.
- NIMH-supported researchers are using biostatistical and machine learning methods to examine long-term outcomes among school-aged children whose autism was detected early between 12-24 months of age compared to children with ASD who did not participate in an early detection program (R01MH121595, R01MH121599).
- NIMH-supported researchers are investigating how best to support providers who work with children with autism who have high service needs in elementary school settings (R34MH123598) and are testing the effectiveness of theater-based programs to enhance social abilities and peer interactions in youth with autism (R01MH114906).
- NIMH-supported researchers are aiming to improve independent functioning and social well-being in transition age youth and adults with ASD (R01MH121438, R01MH121407). NIMH also supports related research on vocational skills and virtual job interview training for transition age youth (R34MH111531, R34MH111491, R34MH111556). In addition, NIMH-supported researchers are working to understand suicidal ideation/behavior, experiences, and outcomes in adolescents and adults with ASD (R21MH125262).
NIH supports genomics research toward advancing understanding of genetic risk factors for ASD.
- NICHD-, NIEHS-, and NINDS-supported researchers estimated that genetic factors account for around 80% of the risk for ASD. Researchers analyzed health information from more than two million people in five countries and followed children from birth through 16 years of age. The authors concluded that variation in the occurrence of ASD is likely due to inherited genetic influences, although gene-environment interactions were not accounted for and remain an important question that needs to be addressed (PMID: 31314057).28
- NIMH- and National Institute of General Medical Sciences (NIGMS)-supported researchers investigated the role of common and rare genetic variations that create risk for ASD (PMID: 36280734).29 These efforts are primarily led by the Psychiatric Genomics Consortium and the Autism Sequencing Consortium.
- NIMH-supported researchers performed RNA-sequencing on tissue samples spanning 11 cortical areas from post-mortem brain samples from individuals with and without ASD. They observed transcriptomic changes, particularly for gene expression affecting excitatory neurons and glia, providing insight into ASD molecular pathology (PMID: 36323788).30
- NIMH- and National Human Genome Research Institute (NHGRI)-supported researchers found that ultra-rare gene variants are enriched in children with autism, contributing to at least 4.5% of autism risk, similar to the risk estimated from mutations that are not inherited from parents (PMID: 34312540).31
- NICHD-supported researchers estimated autism risk for children whose aunts or uncles have ASD. For children with an aunt or uncle with ASD, 3-5% can also be expected to have ASD, compared to about 1.5% of children in the general population. Researchers found that a child whose mother has a sibling with ASD is not more likely to be affected by ASD compared to a child whose father has a sibling with ASD (PMID: 32430199).32
NIH supports research on biomarkers that may be used to detect ASD, identify subtypes of ASD, serve as early indicators of treatment response, and improve clinical research tools for studying ASD.
- NIMH-, NINDS-, NICHD-, and NIDCD-supported ABC-CT investigators are studying an electroencephalogram (EEG) biomarker which measures neural activity associated with face processing, along with an eye tracking measure of social-visual processing (U19MH108206; PMID: 32116579).33
- NINDS-supported researchers are studying whether EEG features identified in infants can predict the likelihood of being diagnosed with ASD (R01NS120986).
- NICHD-supported researchers identified biomarkers in newborns that may signal ASD months or even years before symptoms or diagnosis. Researchers found that 0- to 3-month-old infants who were then diagnosed with autism later in childhood had low levels of the neuropeptide arginine vasopressin in their cerebrospinal fluid (PMID: 32341146).34
- NICHD-, NIMH-, and NINDS-supported researchers found that changes in the brain’s visual areas in infancy may precede autism diagnosis. Researchers found that children who were diagnosed with ASD at 24 months old had differences in the visual processing areas of the brain that were apparent at 6 months old (PMID: 35615814).35
- NIEHS-, NICHD-, and NIMH-supported researchers have identified biomarkers predictive of ASD diagnosis from the use of technologies developed for measuring chemicals in teeth and hair samples (PMID: 36498727; PMID: 36926653).36,37
- NIMH-supported researchers examined the brain activity of adult pairs (one with autism and one without) engaged in social interactions. Adults with autism had reduced activity in the dorsal parietal cortex brain region in response to eye contact compared to partners without autism. The researchers found a relationship between this pattern of neural activity and measured social function, which suggest its potential utility as an enrichment biomarker for stratification into clinical trials (PMID: 36350848).38
- NINDS-supported researchers are developing neuroimaging analysis methods to identify ASD biomarkers that may predict individual response to intervention (R01NS035193).
NIH supports research on understanding the alterations in brain development and the function of physiological systems that lead to ASD with the aim of developing effective, targeted interventions.
- The NIH Convergent Neuroscience initiative encourages researchers to examine links across genes, cells, brain circuits, and behavior to better understand mental disorders. National Center for Advancing Translational Sciences (NCATS)-; National Heart, Lung, and Blood Institute (NHLBI)-; NHGRI-; NIGMS-; and NIMH-supported researchers are studying gene networks to inform the shared mechanisms of ASD and congenital heart disease, which are distinct disorders that often co-occur (P41GM103504, U01MH115747, R01HG009979, R01HL149746, UL1TR001442).
- NINDS-, NIMH-, and NICHD-supported researchers examined reactivity and connectivity in the amygdala (a brain region associated with emotional responses) in children with ASD, with and without co-occurring disruptive behavior disorders, finding that children with ASD and disruptive behavior showed reduced connectivity between the amygdala and vlPFC (ventrolateral prefrontal cortex; a brain region associated with emotion regulation) compared to children with ASD and no disruptive behavior (PMID: 30979647).39
- NINDS- and NIMH-supported researchers found that disruptions to somatosensory neurons (cells that produce touch perception) may contribute to the development of social and other behavioral deficits in ASD mouse models. The researchers also found that treatment with a γ-aminobutyric acid (GABA) receptor agonist that acts directly on somato-sensory neurons reduced tactile overreactivity and rescued brain and behavioral abnormalities in six ASD mouse models (PMID: 31398341).40
- NINDS-funded researchers measured neuronal activity in the prefrontal cortex (a brain region associated with socialization) in mice while they were alone or engaged in social interaction. The researchers found that social behavior elicits increases in correlated neuronal activity, with prefrontal neurons transmitting socialization information. This ability was diminished in mice lacking the Shank3 gene, which is associated with autism (PMID: 33939689).41
- NICHD- and NIMH-supported researchers examined the Early Start Denver Model (ESDM) intervention using an EEG paradigm reflecting neural processes associated with social information processing in children with autism. Children who received ESDM showed alterations in EEG patterns when viewing a familiar person completing an action, which suggest that ESDM may impact neural circuitry related to social cognition (PMID: 34309743).42
NIH supports research on the core features of ASD, including factors affecting social communication and language, and their links to structural and functional differences in the brain.
- NIMH- and NIDCD-supported investigators using functional magnetic resonance imaging (fMRI) and eye tracking methods found that reduced behavioral preference for affective speech, or "motherese," in children with ASD is associated with impaired development of temporal cortical brain systems that normally respond to parental affective speech (PMID: 34980898).43
- NIMH-, NICHD-, National Center for Research Resources (NCRR)-, and NCATS-supported researchers assessed social abilities in a group of adults with autism. The researchers found that some components of social functioning (e.g., understanding non-verbal social skills, ability to participate in social interaction) were highly correlated with each other (PMID: 29341497).44
- NICHD-, NIGMS-, and NCATS-supported researchers found that regular doses of the hormone oxytocin do not overcome deficits in social functioning among children with ASD (PMID: 34644471).45
- NICHD-, NCATS-, and NIMH-supported researchers conducted a clinical trial of the drug arginine vasopressin, which improved social deficits in children with ASD (PMID: 31043522).46
People with certain genetic disorders, such as fragile X syndrome (FXS), tuberous sclerosis (TSC), and Down syndrome, are more likely to have ASD or present ASD-like characteristics. Understanding the biology of these disorders may provide insights into molecular pathways that are commonly affected in ASD.
- The INvestigation of Co-occurring conditions across the Lifespan to Understand Down syndromE (INCLUDE) Project launched in 2018 in support of a congressional directive calling for a trans-NIH research initiative on health and quality-of-life needs for individuals with Down syndrome. INCLUDE is funding a multi-site project starting in 2023 that will develop novel evidence-based screening and diagnostic measures of ASD in toddlers with Down syndrome.
- As part of the NCATS-led Rare Diseases Clinical Research Network, NINDS, NICHD, and NIMH support the Developmental Synaptopathies Consortium, which includes research teams conducting mechanistic studies of genetic conditions related to ASD and intellectual disability, with the aim of identifying shared molecular pathways and potential new therapeutic targets. NINDS-funded investigators enrolled children ages 3-36 months with TSC in a study that revealed a significant relationship between epilepsy, language development, and ASD diagnosis (PMID: 31864941).47
- NINDS-funded researchers found that deletion of the Tsc1 gene in a mouse model impacted the structure and function of dopamine neurons and led to cognitive behavioral deficits (PMID: 31780742).48 Other researchers supported by NINDS, NIGMS, and NIDCD evaluated the use of gene therapy in a mouse model of TSC2 (TSC is caused by mutations to TSC1 or TSC2 genes). Mice given the gene therapy had extended survival rates compared to controls, demonstrating a potential pathway to treat TSC2 lesions (PMID: 33523984).49
- NINDS-supported researchers recently completed the Preventing Epilepsy Using Vigabatrin In Infants with Tuberous Sclerosis Complex trial that tested whether treatment with anti-seizure medication prevents epilepsy development in infants with TSC, improves outcomes, or reduces risk of developing ASD (NCT02849457); a manuscript reporting the trial outcomes is in preparation.
- The Centers for Collaborative Research in Fragile X and FMR1-Associated Conditions ("Fragile X Centers") are funded by NICHD, with additional support from NIMH and NINDS, and aim to accelerate the translation of basic science discovery in FMR1-associated conditions into potential clinical interventions through partnerships between basic and clinical researchers. Researchers have identified EEG biomarkers for humans with FXS and a mouse model of FXS, and both groups responded to baclofen treatment, a medication used to treat muscle spasticity (PMID: 36167501).50
- NINDS-, NICHD-, and NIDCD-supported researchers recently completed a trial testing whether an mGluR5 inhibitor, in combination with an intensive language intervention, can boost language learning in children with FXS (U01NS096767); a manuscript reporting the trial outcomes is under review.
- NINDS- and NICHD-supported researchers used a mouse model of Rett syndrome to show that motor and memory skills training improved performance on motor and memory tasks and delayed symptom onset (PMID: 33762729).51 NINDS-funded researchers also used RNA editing in a mouse model to repair a mutation that causes Rett syndrome (PMID: 32668243).52
On September 26, 2023, the National Institute on Minority Health and Health Disparities (NIMHD) designated people with disabilities as a population with health disparities for research supported by the NIH. In addition, NIH also issued a Notice of Funding Opportunity [Health and Health Care Disparities Among Persons Living with Disabilities (R01 - Clinical Trials Optional) PAR-23-309] calling for research applications focused on novel and innovative approaches and interventions that address the intersecting impact of disability, race and ethnicity, and socioeconomic status on health care access and health outcomes. These actions are part of NIH’s effort to address health disparities faced by people with disabilities and ensure their representation in NIH research.
- Research on Autism Spectrum Disorders (R03 Clinical Trial Optional) PA-21-199
- Research on Autism Spectrum Disorders (R21 Clinical Trial Optional) PA-21-200
- Research on Autism Spectrum Disorders (R01 Clinical Trial Optional) PA-21-201
- Autism Centers of Excellence: Networks (R01 Clinical Trial Optional) RFA-HD-22-007
- Autism Centers of Excellence: Centers (P50 Clinical Trial Optional) RFA-HD-22-008
- Notice of Special Interest: Promoting Language and Communication in Minimally Verbal/ Non-Speaking Individuals with Autism NOT-DC-23-009
In addition to providing funding for autism and disability research, NIH has also hosted several workshops and special events on new and emerging areas of autism- and disability-related research.
- NIA hosted a workshop in March 2022 with presentations on epidemiological and basic science research in ASD and Alzheimer’s disease to explore potential links between the two conditions and identify opportunities for research in this area.
- NIEHS hosted a two-day workshop in June 2022 focused on the possible role of maternal diet and nutrition in mitigating the effects of environmental risks relevant to neurodevelopmental disorders like autism. Speakers discussed a variety of topics, including mechanisms linking maternal nutrition and neurodevelopment, modifiers of environmental exposure, and methods for studying complex nutrient effects.
- NHGRI held a two-day symposium in October 2022 that addressed historical and present-day constructions of disability and ableism, with a focus on the history and lived experiences of people with disabilities in the context of genetics and genomics. Speakers considered how scientific program funding language, including NIH communications, can better address the complexity of disability, health, and wellness.
- NIDCD sponsored a workshop in January 2023 which featured the latest research focused on minimally verbal/non-speaking individuals with autism, as well as research on augmentative and alternative communication (AAC) across populations. As a result of this workshop, NIDCD published a Notice of Special Interest to encourage applications for research to promote language and communication in autistic individuals who are minimally verbal/non-speaking.
- NICHD sponsored a two-day workshop in April 2023 that focused on awareness and research opportunities to mitigate the effects of ableism in both clinical care and the biomedical and behavioral research enterprise.
NIH supports research that addresses all seven Question areas of the IACC Strategic Plan. The NIH Institutes, Centers, and Offices (ICOs) engaged in funding autism research make ongoing efforts to address Objectives of the Strategic Plan that align with the research priorities as defined by their respective ICOs. These efforts are facilitated through regular monthly meetings of the NIH Autism Coordinating Committee (ACC), an internal committee that communicates information about research initiatives and results. The NIH ICOs represented on the ACC include NICHD, NIDCD, NIEHS, NIMH, and NINDS. Staff from the NIMH ONAC and the NIMH Office of Technology Development and Coordination, which manages the NIMH Data Archive (including data collected from participants in autism studies), also participate in NIH ACC meetings. In addition, the NIH Director serves as a statutory member of the IACC, and the directors of NICHD, NIDCD, NIEHS, NIMH, and NINDS are all members of the Committee. The NIMH Director serves as the chair of the IACC. NIH also participates as a member agency of the FIWA. NIH’s research portfolio covers a variety of topics related to autism, including autism etiology, epidemiology, genetics, neurodevelopment, interventions, and screening. NIH also supports professional training and the development of research infrastructure that will facilitate research in ASD and other intellectual and developmental disabilities.
Table 9: FY 2019 – FY 2023 NIH autism funding (thousands of dollars).
| NIH ASD-Related Expenditures by ICO for FY 2019 – FY 2023 (thousands of dollars) | |||||
|---|---|---|---|---|---|
| Participating ICO | FY 2019 Actual | FY 2020 Actual | FY 2021 Actual | FY 2022 Actual | FY 2023 Estimate* |
Participating ICOFIC |
FY 2019 Actual$10 |
FY 2020 Actual$5 |
FY 2021 Actual– |
FY 2022 Actual$106 |
FY 2023 Estimate*N/A |
Participating ICONCATS |
FY 2019 Actual$517 |
FY 2020 Actual$406 |
FY 2021 Actual$654 |
FY 2022 Actual$360 |
FY 2023 Estimate*N/A |
Participating ICONCCIH |
FY 2019 Actual$402 |
FY 2020 Actual$628 |
FY 2021 Actual$515 |
FY 2022 Actual$733 |
FY 2023 Estimate*N/A |
Participating ICONCI |
FY 2019 Actual– |
FY 2020 Actual$58 |
FY 2021 Actual$504 |
FY 2022 Actual$717 |
FY 2023 Estimate*N/A |
Participating ICONEI |
FY 2019 Actual$905 |
FY 2020 Actual$1,084 |
FY 2021 Actual$996 |
FY 2022 Actual$2,697 |
FY 2023 Estimate*N/A |
Participating ICONHGRI |
FY 2019 Actual$866 |
FY 2020 Actual– |
FY 2021 Actual$180 |
FY 2022 Actual$776 |
FY 2023 Estimate*N/A |
Participating ICONIA |
FY 2019 Actual$2,171 |
FY 2020 Actual$732 |
FY 2021 Actual$139 |
FY 2022 Actual$1,585 |
FY 2023 Estimate*N/A |
Participating ICONIAAA |
FY 2019 Actual$250 |
FY 2020 Actual$1,485 |
FY 2021 Actual$2,225 |
FY 2022 Actual$1,680 |
FY 2023 Estimate*N/A |
Participating ICONIAID |
FY 2019 Actual– |
FY 2020 Actual$622 |
FY 2021 Actual$556 |
FY 2022 Actual$623 |
FY 2023 Estimate*N/A |
Participating ICONIAMS |
FY 2019 Actual$492 |
FY 2020 Actual$325 |
FY 2021 Actual$314 |
FY 2022 Actual$343 |
FY 2023 Estimate*N/A |
Participating ICONIBIB |
FY 2019 Actual$228 |
FY 2020 Actual– |
FY 2021 Actual– |
FY 2022 Actual– |
FY 2023 Estimate*N/A |
Participating ICONICHD |
FY 2019 Actual$37,848 |
FY 2020 Actual$37,809 |
FY 2021 Actual$38,218 |
FY 2022 Actual$38,906 |
FY 2023 Estimate*N/A |
Participating ICONIDA |
FY 2019 Actual$977 |
FY 2020 Actual$967 |
FY 2021 Actual– |
FY 2022 Actual$1,335 |
FY 2023 Estimate*N/A |
Participating ICONIDCD |
FY 2019 Actual$15,923 |
FY 2020 Actual$15,653 |
FY 2021 Actual$14,020 |
FY 2022 Actual$17,172 |
FY 2023 Estimate*N/A |
Participating ICONIDCR |
FY 2019 Actual$722 |
FY 2020 Actual$716 |
FY 2021 Actual$588 |
FY 2022 Actual$465 |
FY 2023 Estimate*N/A |
Participating ICONIEHS |
FY 2019 Actual$11,647 |
FY 2020 Actual$15,031 |
FY 2021 Actual$10,419 |
FY 2022 Actual$12,540 |
FY 2023 Estimate*N/A |
Participating ICONIGMS |
FY 2019 Actual$4,587 |
FY 2020 Actual$4,548 |
FY 2021 Actual$5,155 |
FY 2022 Actual$4,962 |
FY 2023 Estimate*N/A |
Participating ICONIMH |
FY 2019 Actual$161,304 |
FY 2020 Actual$164,347 |
FY 2021 Actual$162,219 |
FY 2022 Actual$166,116 |
FY 2023 Estimate*N/A |
Participating ICONINDS |
FY 2019 Actual$24,088 |
FY 2020 Actual$29,363 |
FY 2021 Actual$31,937 |
FY 2022 Actual$32,883 |
FY 2023 Estimate*N/A |
Participating ICOOD |
FY 2019 Actual$18,170 |
FY 2020 Actual$15,153 |
FY 2021 Actual$16,032 |
FY 2022 Actual$17,273 |
FY 2023 Estimate*N/A |
Participating ICONIH Roadmap for Medical Research |
FY 2019 Actual$7,769 |
FY 2020 Actual$3,896 |
FY 2021 Actual$1,508 |
FY 2022 Actual$3,213 |
FY 2023 Estimate*N/A |
Participating ICONLM |
FY 2019 Actual$1,240 |
FY 2020 Actual$1,212 |
FY 2021 Actual$1,684 |
FY 2022 Actual$1,984 |
FY 2023 Estimate*N/A |
Participating ICOTotal NIH |
FY 2019 Actual$290,117 |
FY 2020 Actual$294,039 |
FY 2021 Actual$287,860 |
FY 2022 Actual$306,470 |
FY 2023 Estimate*$319,000 |
Table shows NIH expenditures on ASD, as reported through the NIH Research Portfolio Online Reporting Tool (NIH RePORT) for estimates of funding for various Research, Condition, and Disease Categories (RCDC).
* FY 2023 data have not been finalized in RePORT RCDC, and total NIH FY 2023 data are estimates based on the FY 2022 actual.
Table 10: FY 2019 – FY 2022 NIH funding of the ACE program, which incudes centers (P50) and cooperative agreements (U01).
| NIH ACE Program Expenditures for FY 2019 – FY 2022 (thousands of dollars) | ||||
|---|---|---|---|---|
| Participating ICO | FY 2019 | FY 2020 | FY 2021 | FY 2022 |
Participating ICONIDCD |
FY 2019$150 |
FY 2020$150 |
FY 2021$150 |
FY 2022$400 |
Participating ICONICHD |
FY 2019$10,337 |
FY 2020$10,433 |
FY 2021$10,038 |
FY 2022$10,350 |
Participating ICONIMH |
FY 2019$11,560 |
FY 2020$11,038 |
FY 2021$10,983 |
FY 2022$9,010 |
Participating ICONINDS |
FY 2019$531 |
FY 2020$933 |
FY 2021$933 |
FY 2022$1,500 |
Participating ICONIEHS |
FY 2019$250 |
FY 2020$250 |
FY 2021$245 |
FY 2022$2,011 |
Participating ICOTotal NIH |
FY 2019$22,958 |
FY 2020$22,904 |
FY 2021$22,382 |
FY 2022$23,270 |
Office of the Assistant Secretary for Planning and Evaluation (ASPE)
The Assistant Secretary for Planning and Evaluation (ASPE) is the principal advisor to the HHS Secretary on policy development and is responsible for major activities in policy coordination, legislation development, strategic planning, policy research, evaluation, and economic analysis. The Office of Behavioral Health, Disability, and Aging Policy (BHDAP) within ASPE focuses on policies and programs that support the independence, productivity, health and well-being, and long-term care needs of people with disabilities, older adults, and people with mental and substance use disorders. The Division of Disability and Aging Policy is responsible for the analysis, coordination, research, and evaluation of policies related to mental and substance use disorders and is the focal point for policy development and analysis related to the financing, access/delivery, organization, and quality of services for adults and children with mental and substance use disorders, including those with co-occurring developmental disabilities such as ASD. The following initiatives, projects, and programs are related to autism but are not specifically in place to implement the Autism CARES Act of 2019.
In 2021, ASPE published the report Health Insurance Coverage Among Working Age Adults with Disabilities, which tracked changes in health insurance coverage for this population from 2010-2019. From 2010-11 to 2017-18, the proportion of U.S. adults with disabilities who lacked health insurance coverage for a full year was nearly halved, falling by about 46% from 17% to 9%. There was also an increase of about 14% in the proportion of adults with disabilities who had continuous coverage, from about 71% to 81%. These improvements were concentrated immediately after 2014, when the largest Affordable Care Act (ACA)-driven insurance expansions first took effect. Coverage gains were particularly large for Medicaid, coinciding with the ACA’s Medicaid expansion program that took effect in most states starting in 2014. Having coverage for only part of the year, however, remained more than 50% more common for adults with disabilities (10% in 2017-18) than those without disabilities (6% in 2017-18) throughout the study period. The American Rescue Plan Act of 2021 expanded subsidies for Marketplace plans (since extended through 2024 under the Inflation Reduction Act), which has the potential to increase coverage further for adults with disabilities. An estimated 532,000 uninsured adults with disabilities (about 67%) now have access to a zero-premium plan after premium tax credits on Healthcare.gov, an increase of 16.8% points from pre-American Rescue Plan estimates.
In response to the coronavirus pandemic, ASPE published an issue brief on Child and Adolescent Mental Health During COVID-19, which identifies children with disabilities among the most disproportionately affected by a mental health condition during COVID-19 and describes policy considerations for schools and early childhood service providers. ASPE also published a report on COVID-19 and People with Intellectual and Developmental Disabilities to examine state collection and reporting of COVID-19 data, COVID-19 infection prevention strategies, and COVID-19 vaccine prioritization for the intellectual and developmental disability population at the state level to help inform future policies, programs, and practices that aim to reduce the risk of infection and mitigate adverse effects of COVID-19 and other infectious diseases for the population.
ASPE published an issue brief in 2022 entitled Improving Data Infrastructure for Patient-Centered Outcomes Research for People with Intellectual and Developmental Disabilities, which describes insights gained from key informant interviews and a listening session on short-term opportunities to improve patient-centered outcomes research data infrastructure relevant to people with intellectual and developmental disabilities.
ASPE, in collaboration with a researcher at Atrium Health, conducted an analysis on psychotropic medication use and co-occurring mental health and developmental disabilities among children and adolescents with FASDs. The data for the study came from the 2017 IBM Watson Health MarketScan Multistate Medicaid and Commercial Claims database, a large, national dataset of Medicaid and commercial claims. The sample for the analysis includes children between the ages of 0 and 17 with either FASDs diagnosis or a mental health diagnosis (N=5,848,721 Medicaid; N=5,511,061 private insurance). ASD was a concurrent condition in 22% of children with FASDs on psychotropic medication with private insurance and 26% among those with Medicaid. There are studies with small sample sizes showing autistic traits in individuals with prenatal alcohol exposure, but this is the first large population-based study in the United States showing the prevalence of ASD diagnosis among children with FASDs. This analysis was published in the journal Pediatrics in 2022.53
ASPE authored the manuscript Psychotropic Medication and Psychosocial Service Use among Individuals with Autism Spectrum Disorder. Using national multi-payer claims data, the study estimates a multinomial logistic regression model to discern psychotropic medication and psychosocial service use among transition age youth with ASD (12-26 years; N=52,083) compared to a matched cohort of those without ASD (12-26 years; N=52,083). Approximately one third of transition age youth with ASD and no mental health condition receive only psychotropic medication, and the likelihood of using both psychosocial services and medication is higher only when transition age youth with ASD have a co-occurring mental health condition. The manuscript was accepted by the American Journal on Intellectual and Developmental Disabilities for publication.
ASPE continued work on the Integrated Dataset on Intellectual and Developmental Disabilities, a linked dataset which will enable researchers to analyze relationships between various sociodemographic information, need for HCBS, service utilization, service expenditures, and person-centered outcomes prior to and during the COVID-19 pandemic for individuals with intellectual and developmental disabilities, including ASD. The project includes an inter-departmental technical expert panel led by ASPE/BHDAP, with representatives from HHS [ACL’s AoD and NIDILRR, CDC’s NCBDDD, NIH’s NICHD and NIMH, CMS’s Office of Minority Health and Center for Medicaid & CHIP Services] and DOL [Office of Disability Employment Policy (ODEP)].
ASPE and Mathematica started the research project Innovative 988 Crisis Services Systems for Children, Youth, and People with Disabilities. The purpose of this project is to expand ASPE’s current research on the 988 crisis services system and explore innovative 988 systems that integrate service systems beyond law enforcement and emergency medical services (e.g., education, child welfare, developmental disabilities) to effectively provide 988 crisis, stabilization, and recovery oriented supports and services for children, youth, and people with disabilities (e.g., Alzheimer’s disease and related dementias, intellectual and developmental disabilities).
While ASPE does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, research and analyses conducted by ASPE are relevant to individuals with disabilities, including those on the autism spectrum and their families. These projects are intended to guide policy development and coordination to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. ASPE activities are also relevant to Question 4 (Interventions), Question 5 (Services and Supports), Question 6 (Lifespan), and Question 7 (Infrastructure and Prevalence) of the IACC Strategic Plan. ASPE is a member of the FIWA and participates in efforts to coordinate autism activities across the federal government.
Substance Abuse and Mental Health Services Administration (SAMHSA)
The mission of the Substance Abuse and Mental Health Services Administration (SAMHSA) is to lead public health and service delivery efforts that promote mental health, prevent substance misuse, and provide treatments and supports to foster recovery while ensuring equitable access and better outcomes. SAMHSA accomplishes this mission by providing behavioral health leadership and resources, program funding, policies, information and data, and technical assistance.
While SAMHSA does not receive funding from and is not directly involved in implementing the Autism CARES Act of 2019, several SAMHSA programs support individuals who have been diagnosed with ASD and co-occurring serious emotional disturbances (SEDs), serious mental illnesses (SMIs), and/or substance use disorders (SUDs). However, it is important to note that some individuals who are diagnosed with ASD may not be diagnosed with SED, SMI, or SUD. Additionally, while individuals with ASD may have different ways of learning, moving, or paying attention, these characteristics may also appear in individuals not on the autism spectrum. ASD is a neurodevelopmental disability, not a mental disorder, and it is not considered an SMI.
Since 1993, SAMHSA has implemented the Children’s Mental Health Initiative (CMHI). CMHI prepares children and young adults (birth through 21) who are at risk for or meet criteria for SED, including some children and youth on the autism spectrum, for successful transitions to adulthood and assumption of adult roles and responsibilities. This initiative provides funds to public entities to create "systems of care," which are defined as a spectrum of effective, community-based services and supports for children and youth with or at risk for mental health or other challenges and their families that is organized into a coordinated network, builds meaningful partnerships with families and youth, and addresses their cultural and linguistic needs in order to help them to function better at home, in school, in the community, and throughout life. In FY 2022, CMHI systems of care served 9,485 individuals with SMI or SED diagnoses. Of those enrolled, 54.1% reported positive functioning in everyday life at 6-month follow-up, and 79% were attending school regularly. In addition to direct service care, this grant program trained 24,067 individuals in the mental health and related workforce in specific mental health-related practices and activities.
SAMHSA implemented the CMHI Clinical High Risk for Psychosis (CHR-P) Program in 2018 to support youth and young adults (not more than 25 years of age) who are identified to be at clinical high risk for developing a first episode of psychosis. CHR-P served 664 youth and young adults at clinical high risk for psychosis. Of those enrolled, 66.1% reported positive functioning in everyday life at 6-month follow-up, and 84.8% were attending school regularly and/or currently employed. In addition to direct service care, CHR-P screened 8,560 individuals for mental health and related interventions. CHR-P provided outreach to 17,424 individuals and made 5,873 referrals to mental health or related services.
SAMHSA funds the Substance Use Prevention, Treatment, and Recovery Services Block Grant (SUBG) and the Community Mental Health Services Block Grant (MHBG) to states. The FY 2024 – FY 2025 Block Grand Application and Plan emphasizes the importance of interagency collaboration and support for local early childhood behavioral health efforts. In the Block Grant, children with SED refers to persons from birth to age 18. The Block Grant includes support for recovery services as well as primary prevention activities.
The SUBG supports services such as primary prevention and early intervention for those with human immunodeficiency virus/acquired immune deficiency syndrome, services for substance-using pregnant women and dependent children, and support for persons who inject drugs. States and jurisdictions receiving this Block Grant admitted 1,761,772 clients in FY 2022.
The MHBG supports those with SMIs, including schizophrenia and bipolar disorder. Activities supported through the MHBG include supported housing, supported employment, peer services, wraparound services for children, outpatient services, and crisis stabilization and management. The MHBG requires a 10% set aside for early SMI, including psychotic disorders. The Block Grant also requires a 10% set aside for crisis services. Block Grant recipients report client-level data based on National Outcome Measures. In 2021, the Block Grant program served 5.986 million adults and 2.209 million children.
SAMHSA also funds Project AWARE (Advancing Wellness and Resiliency in Education), which seeks to develop collaborations among state mental health authorities, local education agencies, behavioral health providers, and those serving youth. The program may offer supports to students with behavioral health conditions, including ASD, to help students engage and participate in school settings and interact with peers. In FY 2022, Project AWARE grantees trained 252,498 individuals in mental health and related practices, screened 254,001 children and youth for mental health related concerns, and referred 62,748 children and youth for mental health services and treatment.
SAMHSA’s Healthy Transitions: Improving Life Trajectories for Youth and Young Adults with Serious Mental Disorders Program is intended to improve access to mental health treatment and support for young people aged 16 to 25 who have or are at risk of developing serious mental health conditions. Some young adults with ASD, along with others with behavioral health conditions, may benefit from the extra supports and services offered by this program to navigate the social contexts, physical changes, and developmental changes during this transition age period. In FY 2022, nearly 3,200 youth and young adults were served by the Healthy Transitions grant program, with youth and young adults reporting enhanced social connectedness, absence of psychological distress, and ability to attend school or obtain employment.
SAMHSA’s Project LAUNCH (Linking Actions for Unmet Needs in Children's Health) seeks to promote the wellness of young children, from birth to 8 years of age, by addressing the social, emotional, cognitive, physical, and behavioral aspects of their development, preparing young children to thrive in school and beyond. Strategies include training, referrals, and treatment. More than 250,000 children have been screened and referred for services under this program, which became a national initiative in 2008. Early interventions and supports offered by this program for young children and their families may help prevent disruptions to family life, help families bond, and promote acceptance of a child with a disability, including ASD. In FY 2022, LAUNCH grantees trained roughly 6,330 people in mental health-related work-force activities, screened roughly 17,450 children for mental health services, and referred roughly 5,580 children for mental health or related services.
SAMHSA also supports the Mental Health Technology Transfer Center (MHTTC) Network. This program may conduct trainings or webinars on topics such as intellectual and developmental disabilities, including ASD, or seclusion and restraint. The MHTTC includes 10 Regional Centers, a National American Indian and Alaska Native Center, a National Hispanic and Latino Center, and a Network Coordinating Office. MHTTC grantees may collaborate with SAMHSA’s other technical assistance providers, including those focusing on SUD prevention and treatment. In FY 2022, the MHTTCs conducted 986 trainings and technical assistance activities for nearly 52,000 individuals.
SAMHSA’s Criminal and Juvenile Justice Programs help to support early intervention and diversion for youth and young adults with behavioral health conditions who come into contact with the criminal justice system. This includes support for the GAINS (Gather, Assess, Integrate, Network, and Stimulate) Center for Behavioral Health and Justice Transformation which provides technical support to communities and professionals to support persons with behavioral health conditions in the criminal justice system, including diversion approaches.
SAMHSA additionally supports the National Child Traumatic Stress Initiative and the National Child Traumatic Stress Network (NCTSN). This program supports a network of 184 centers and 200 affiliates, including hospitals, universities, and community organizations. The NCTSN previously published a toolkit in 2015 to support delivery of a training for mental health and other professionals on supporting children with intellectual and developmental disabilities in coping with and recovering from trauma. In 2021, the Network held three webinars on building resilience and tailoring trauma-focused cognitive behavioral therapy (CBT) for children with intellectual and developmental disabilities. NCTSN grantee sites provided trauma-informed training to over 326,177 people in FY 2022.
SAMHSA also funds the Protection & Advocacy for Individuals with Mental Illness (PAIMI) Program, which is intended to protect and advocate for the rights of adults with SMI and children with SED. Additionally, the PAIMI biennial report is included in the Appendix to the Secretary’s biennial report on federal disability activities, which is prepared by ACL. In the most recent 2019 and 2020 PAIMI Activities Report, there were several PAIMI cases related to individuals with autism and co-occurring SMI/SED.
SAMHSA also administers the Evidence-Based Practices Resource Center (EBPRC), which develops products relevant to children and youth, including those with developmental disabilities such as autism. In 2021, the EBPRC developed a guide on Treatment Considerations for Youth and Young Adults with Serious Emotional Disturbances and Serious Mental Illnesses and Co-occurring Substance Use.
SAMHSA’s Strategic Prevention Framework – Partnerships for Success and Strategic Prevention Framework for Prescription Drugs (SPF-Rx) support efforts to address underage drinking, marijuana use, and prescription drug misuse among adolescents and young adults; raise awareness about the dangers of sharing medications, as well as the risks of fake or counterfeit pills purchased over social media or other unknown sources; and work with pharmaceutical and medical communities on the risks of overprescribing among those 18 years of age and older. The SPF-Rx program assists grantees in developing capacity and expertise in leveraging data from state-run prescription drug monitoring programs to reduce opioid misuse, opioid use disorder, and overdose death. Funded grantees have reported reductions in opioid misuse and overdoses.
While not specific to persons with developmental disabilities, SAMHSA supports programs to facilitate use of telehealth services when feasible and appropriate, which can help to expand access to services. SAMHSA has also worked with CMS to develop guidance on school-based health services and Medicaid. SAMHSA additionally works to promote youth, school/campus, and family engagement in services and programs. SAMHSA promotes culturally competent programs for ethnic, racial, and LGBTQIA+ populations through the Office of Behavioral Health Equity (OBHE). SAMHSA’s OBHE and Office of Tribal Affairs and Policy also support the needs of American Indian and Alaska Native populations. SAMHSA recently developed a guide to support evidence-based practices in under-resourced populations, and SAMHSA supports the National Network to Eliminate Disparities in Behavioral Health.
SAMHSA also supports the Early Serious Mental Illness Treatment Locator, which helps individuals, families, and providers find treatment facilities and programs that support persons with first onset of SMIs such as psychosis and schizophrenia. Other services locators also can help persons with developmental disabilities and behavioral health conditions locate treatment options, including maps and directories of programs offering mental health and SUD treatment, including hotlines such as the 988 Suicide & Crisis Lifeline.
SAMHSA additionally supports the Projects for Assistance in Transition from Homelessness (PATH) program, which funds services for people with SMI experiencing homelessness. PATH supports outreach, screening, and referral to housing, employment, and other services. PATH includes grants to states and territories and was originally authorized by the Stewart B. McKinney Homeless Assistance Amendments Act of 1990 and has been authorized most recently by the Consolidated Appropriations Act, 2023. In addition, SAMHSA supports education and employment programs for persons with behavioral health conditions, including those with developmental disabilities such as ASD. For example, SAMHSA’s Supplemental Security Income (SSI)/Social Security Disability Insurance (SSDI) Outreach, Access, and Recovery program supports enrollment into SSI and SSDI for eligible persons with behavioral health conditions, including ASD.
While SAMHSA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services provided by SAMHSA are relevant to individuals with behavioral health conditions, including those on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. SAMHSA activities are also relevant to Question 4 (Interventions), Question 5 (Services and Supports), and Question 6 (Lifespan) of the IACC Strategic Plan. SAMHSA is a member of the IACC and the FIWA and participates in efforts to coordinate autism activities across the federal government.
Department of Defense (DOD)
The U.S. Department of Defense (DoD) is charged with coordinating and supervising all agencies and functions of the government concerned directly with national security and the U.S. Armed Forces. This section provides an overview of the ASD-related research, services, and support activities of the Army, the Military Health System (MHS)/TRICARE, and the Defense Advanced Research Projects Agency (DARPA).
Army
The DoD Autism Research Program (ARP) was first established through language in the 109th U.S. Congress, House of Representative Conference Report (H.R. 5631) in FY 2007 with an appropriation of $7.5 million for research on ASD in the military. Following in FY 2008 through FY 2023, the DoD ARP has continued through the Defense Health Program with additional appropriations. From FY 2007 to FY 2023, a total of $149.4 million has been designated for research into ASD through an addition to the DoD appropriation bill. This program is not authorized or funded through the Autism CARES Act of 2019.
The ARP is a partnership between the DoD, researchers, and consumers. The vision and mission of the ARP has been to improve the lives of individuals with ASD now and in their future by promoting innovative research that advances the understanding of ASD and leads to improved outcomes. This sense of urgency has resulted in funding research aimed at having an immediate impact on those with ASD. Funded projects span the continuum of research – from biological mechanisms of ASD to interventions focused on improving treatment and health outcomes, quality of life, and promoting community inclusion for those living with ASD.
The ARP funds research projects across many of the strategic priorities outlined in the IACC Strategic Plan. Many of the ARP’s Areas of Interest encompass IACC priorities. The program continues to invest heavily in research addressing the following areas of the IACC Strategic Plan: Question 2 (Biology), Question 3 (Genetic and Environmental Factors), Question 4 (Interventions), Question 5 (Services and Supports), and Question 6 (Lifespan). In addition, DoD is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Table 11: Appropriations for and number of awards funded through the ARP for FY 2019 – FY 2023.
| DoD Autism Research Program Appropriations and Awards: FY 2019 – FY 2023 | ||
|---|---|---|
| Fiscal Year | Appropriation | Awards Funded |
Fiscal Year2019 |
Appropriation$7.5 million |
Awards Funded8 |
Fiscal Year2020 |
Appropriation$15 million |
Awards Funded12 |
Fiscal Year2021 |
Appropriation$15 million |
Awards Funded14 |
Fiscal Year2022 |
Appropriation$15 million |
Awards Funded11 |
Fiscal Year2023 |
Appropriation$15 million |
Awards FundedN/A |
Information on the number of awards funded in FY 2023 was not available at the time this report was written.
Military Health System (MHS)/TRICARE
TRICARE is the worldwide DoD health care program serving 9.6 million service members (Active and Guard/Reserve) on Active Duty (greater than 30 days) and their families, as well as retirees, their families, survivors, and certain former spouses. As a major component of the Military Health System (MHS), TRICARE brings together the military hospitals and clinics worldwide (often referred to as "direct care," military medical treatment facilities, and military dental treatment facilities) with network and non-network TRICARE-authorized civilian health care professionals, institutions, pharmacies, and suppliers (often referred to as "private sector care") to provide access to the full array of high-quality health care services while maintaining the capability to support military operations. The MHS includes physician and other licensed independent provider services, pharmacy coverage, psychosocial treatment, psychological testing, occupational therapy, physical therapy, and speech and language pathology for the treatment of ASD to all eligible TRICARE beneficiaries under the TRICARE Basic Program, which is the medical benefit plan of the MHS. A separate but related TRICARE program, the Extended Care Health Option (ECHO), offers supplemental services to Active Duty Family Members with a qualifying physical or psychologically disabling condition, including ASD.
ABA services are currently offered under the TRICARE Comprehensive Autism Care Demonstration (ACD) in accordance with the Defense Health Agency (DHA)’s separate (and limited) demonstration authority found in the U.S.C., Title 10, Section 1092, as implemented by the Code of Federal Regulations, Title 32, Section 199.1(o). DHA is the responsible entity within the DoD for the ACD. The ACD began on July 24, 2014, and is currently authorized through December 31, 2028. Information regarding the ACD policy can be found in the TRICARE Operations Manual.
The DHA does not receive any funding from the Autism CARES Act of 2019. Table 12 details the health care costs in FY 2019 – FY 2021 for ACD-participating beneficiaries for the ABA services authorized under the ACD. Over the course of the demonstration, the DHA has hosted various round table and information sessions for interested stakeholders including, but not limited to, ABA providers, Active Duty military providers, advocates, families, and congressional staff. Additionally, current ACD initiatives include TRICARE quality management audits, outcome measures, parent surveys, and DoD Office of the Inspector General audits. The Department also published a policy update in 2021 that included a number of improvements to the ACD, including enhanced support to parents and caregivers, improved care coordination, and ensuring that services are directed to those beneficiaries who will benefit the most, with the focus always on helping military beneficiaries diagnosed with ASD, and their families, to reach their maximum potential.
Table 12: Health care costs for ACD-participating beneficiaries for the ABA services authorized under the ACD for FY 2019 – FY 2021.
| Costs for ABA Services Authorized under the ACD: FY 2019 – FY 2021 | ||
|---|---|---|
| Fiscal Year | Appropriation | Awards Funded |
Fiscal Year2019 |
Appropriation$376.1 million |
Awards Funded16,001 |
Fiscal Year2020 |
Appropriation$399.4 million |
Awards Funded16,312 |
Fiscal Year2021 |
Appropriation$454.5 million |
Awards Funded16,677 |
Information for FY 2022 and FY 2023 was not available at the time this report was written.
In addition to medical services covered under the TRICARE Basic medical benefit, covered ECHO benefits, and the ACD, DoD also offers non-medical services through the Exceptional Family Member Program (i.e., non-medical respite) and Military OneSource (i.e., non-medical counseling and non-clinical resources) to support beneficiaries including those with a diagnosis of ASD and their family members.
The DHA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, and the DHA’s authority for coverage is separate and distinct from the IACC and the Autism CARES Act of 2019. The DHA monitors the efforts of the IACC, to include the contents of the IACC Strategic Plan, and services provided by DHA are relevant to individuals with disabilities, including individuals on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. DHA activities are also relevant to Question 4 (Interventions) and Question 5 (Services and Supports) of the IACC Strategic Plan. TRICARE is a member of the FIWA and participates in efforts to coordinate autism activities across the federal government.
Defense Advanced Research Projects Agency (DARPA)
The Defense Advanced Research Projects Agency (DARPA) serves as the central research and development organization of the DoD and seeks to make pivotal investments in breakthrough technologies for national security. The Physics of Artificial Intelligence (PAI) research program was part of a broad DARPA initiative to develop and apply "Third Wave" artificial intelligence (AI) technologies to sparse data and adversarial spoofing and incorporate domain-relevant knowledge through generative contextual and explanatory models. PAI aimed to show that embedding physics and prior knowledge into AI will help to overcome the challenges of sparse data and facilitate the development of generative models that are causal and explanative.
Through PAI, DARPA funded investigators at the University of Chicago from 2018 to 2021 to investigate, develop, and implement tools to augment current machine learning tools and capabilities. The research group applied their PAI work to a variety of areas, including ASD and the need for tools that help identify children with ASD as early as possible. The group developed and validated machine inferred digital biomarkers for autism using individual diagnostic codes already recorded during medical encounters.54 Their risk estimator identifies children at high risk from shortly after 2 years of age for either sex and across two independent databases of patient records. They systematically leverage ASD comorbidities, with no requirement of additional blood work, tests, or procedures, to compute the Autism Comorbid Risk Score (ACoR), which predicts elevated risk during the earliest childhood years when interventions are the most effective. They concluded that, if adopted in practice, ACoR could significantly reduce the median diagnostic age for ASD and reduce long post-screen wait times experienced by families for confirmatory diagnoses and access to evidence-based interventions.
DARPA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan. However, DARPA has supported research on autism that is relevant to Question 1 (Screening and Diagnosis) of the IACC Strategic Plan. Though DARPA is not currently a member of the IACC or the FIWA, DARPA participates in efforts to coordinate autism activities across the federal government and contributed to this report and the most recent IACC Portfolio Analysis Report.
Department of Education (ED)
The mission of the U.S. Department of Education (ED) is to promote student achievement and preparation for global competitiveness by fostering educational excellence and ensuring equal access. ED supports programs to develop and implement evidence-based practices for services to youths and postsecondary students, as well as programs for individuals with disabilities who have graduated from high school or a postsecondary institution and are seeking vocational rehabilitation (VR) services. ED supports ASD-related services, supports, and research through programs administered by ED’s Institute of Education Sciences (IES) and the Office of Special Education and Rehabilitative Services (OSERS). An overview of these programs is provided below.
Institute of Education Sciences (IES)
The Institute of Education Sciences (IES) is the independent research, evaluation, and data collection arm of ED. IES’s mission is to provide scientific evidence on which to ground education practice and policy and to share this information in formats that are useful and accessible to educators, parents, policymakers, researchers, and the public. Each of the four IES Centers supports work related to ASD. The programs and projects administered by the four IES Centers are described below.
The National Center for Special Education Research (NCSER) funds research on ASD primarily under the Special Education Research Grants Program (84.324A). This program supports research on comprehensive interventions that target multiple coordinated outcomes, as well as targeted interventions focused on a single outcome (such as social communication). Studies funded under this program examine children with or at risk for ASD from infancy through postsecondary education. Additional research projects on ASD have been funded through Research Training Programs in Special Education; Special Education Research and Development (R&D) Centers; Low-Cost, Short-Duration Evaluation of Special Education Interventions; and unsolicited grant opportunities. In 2012, as part of the R&D Centers competition, NCSER funded the Center on Secondary Education for Students with Autism Spectrum Disorders (CSESA) to develop and test a comprehensive, school-based intervention to improve the cognitive, communicative, academic, social, behavioral, functional, and transition outcomes of secondary students with ASD. CSESA also disseminated information regarding evidence-based practices and reviews of research. Between FY 2012 and FY 2023, NCSER has funded 71 research projects related to improving outcomes for students with ASD for a total of approximately $110 million in funding.
In June 2021, NCSER announced a new Research to Accelerate Pandemic Recovery in Special Education competition to consider applications that directly address a problem, issue, program, policy, or practice that is related to the COVID-19 pandemic; important to a state or local education agency; has the potential to improve outcomes significantly and rapidly for students with or at risk for disabilities; and will provide actionable and timely results to districts and schools. One of the 2022 grants focused on reducing the time to autism diagnosis for toddlers in early intervention programs (R324X220088). In November of 2021, NCSER announced a new partnership with NSF to fund projects related to AI-Augmented Learning for Individuals with Disabilities. The resulting funded project (2229873) will harness AI technology to support speech-language pathologists (SLPs) working in school settings. This technology will use cutting-edge methods to identify students with speech and language needs and to help SLPs create and deliver individualized language interventions. Though this project does not exclusively focus on autistic learners, findings related to improving in-school speech and language services are relevant to their needs.
Through the Special Education Studies and Evaluation program, the National Center for Education Evaluation and Regional Assistance (NCEE) supports large-scale studies focused on children or youth with disabilities, including those with ASD. The National Longitudinal Transition Study 2012 provides information about the characteristics, school experiences, and outcomes of a nationally representative sample of more than 17,000 youths with disabilities (ages 13-21), including about 1,600 youth in the autism disability category. This study will link the survey information collected in 2012 and 2013 to newly obtained administrative data to follow the youth sample beyond high school. These administrative data include: (1) high school course-taking and completion from district records and (2) postsecondary information from the National Student Clearinghouse and ED’s Federal Student Aid records. NCEE expects to release the next report from this study in 2024.
Through the IDEA State and Local Implementation Study, NCEE will provide a national picture of state, district, and school implementation of the IDEA across the 2019-2020 school year. For this study, NCEE surveyed administrators from all 50 states, the District of Columbia, and territories receiving IDEA funding, as well as a nationally representative sample of school districts and schools. Beginning in 2024, NCEE plans to release findings in a series of topic reports that will likely include a description of practices for identifying students in the autism disability category and the hiring/retention of staff who primarily serve these students.
The National Center for Education Statistics (NCES) conducts longitudinal surveys as part of its mission to collect and analyze data related to education in the United States. The Early Childhood Longitudinal Study, Kindergarten Class of 2010-11 (ECLS-K:2011), is a part of a series of longitudinal studies supported by NCES that provide information about children’s cognitive, social, emotional, and physical development, as well as their home environment, educational activities, school and classroom environment, classroom curriculum, and before- and after-school care. This study included a nationally representative sample of kindergartners selected from public and private schools in 2010-11 who were followed through fifth grade. Approximately 4,920 students had been reported by their parents as diagnosed with a disability by the end of the study, with approximately 180 of these students reported by their parents as having a diagnosis of developmental delay and approximately 240 of these students reported by their parents as having a diagnosis of autism. The next ECLS program study will be the Early Childhood Longitudinal Study, Kindergarten Class of 2023-24 (ECLS-K:2024); data will be available on students with disabilities,* including ASD diagnoses, with the first data release expected in 2025.
The Middle Grades Longitudinal Study (MGLS:2017) was the first study conducted by the NCES to follow a national sample of students from sixth to eighth grade. It collected information on a cohort of sixth graders in 2018 and then collected information on these same students again in 2020. Data were collected on this cohort of students’ academic, social, and interpersonal status and growth as they transitioned from elementary school and then prepared to enter high school. Direct and indirect assessments of mathematics, reading, and executive function, as well as direct and indirect assessments of socioemotional development, were included. Information was also collected from the students’ parents or guardians, their teachers, and their school administrators. MGLS:2017 field staff provided additional information about the school environment through an observational checklist. The base year data collection specifically oversampled students in the Autism and Emotional Disturbance IDEA categories, obtaining data for more than 600 students with autism in 2018, and almost 400 students that were followed in the 2020 year. The response rate for these collections were low presumably in part because many schools were uncomfortable sharing student disability status as part of this voluntary collection. For this reason, the oversample effort was abandoned for the 2020 sample refresh. Thus, MGLS:2017 is not able to support official statistics for many analyses and is released as restricted-use only data. Regardless of this limitation, variables that call out autism specifically can be used as control or filtering variables for a variety of exploratory research questions. Additionally, special education students have teacher-reported data that may be used in conjunction with other MGLS:2017 data, such as direct assessment math and reading scores. In sum, the MGLS:2017 data offers interesting possibilities for researchers interested in ASD.
The High School Longitudinal Study of 2009 (HSLS:09) is the fifth in a series of high school longitudinal studies conducted by NCES since the 1970s. HSLS:09 focuses on understanding students’ trajectories from the beginning of high school into higher education and the workforce. The core research questions for the study explore secondary to postsecondary transition plans and the evolution of those plans; the paths into and out of science, technology, engineering, and mathematics fields of study and careers; and the educational and social experiences that are related to these shifts in plans or paths. HSLS:09 is a longitudinal study of a nationally representative sample of approximately 23,000 ninth graders from 944 public and private schools. By the most recent survey round in 2016, hundreds of HSLS:09 sample members reported being (or had been reported by their parents to have been) diagnosed with a learning disability, including autism. Approximately 200 of these students were reported by their parents as having a diagnosis of autism in the ninth grade. The High School and Beyond Longitudinal Study of 2022 (HS&B:22) is the next high school cohort to collect disability information such as autism diagnoses. The study began with a ninth-grade cohort in the fall of 2022 and is expected to release initial data in 2024.
* IDEA Part B, 20 U.S.C. § 1401(3), and Part C, 20 U.S.C. § 1432(5), include specific definitions for a “child with a disability” and “an infant or toddler with a disability,” respectively. Additionally, the protections of Section 504, 29 U.S.C. § 794, extend only to individuals who meet the regulatory definition of a person with a disability under 34 C.F.R. 104.3(j). To the extent that the term “students with disabilities” is used throughout this document, it encompasses all students contemplated under the aforementioned sections of the IDEA and Section 504.
The National Center for Education Research (NCER) supports the Department’s Small Business Innovation Research (SBIR) program, which funds the development and testing of education technology products to improve education outcomes. One priority area within the SBIR program focuses on improving outcomes for children with or at risk for disability. As part of this priority area, NCER has supported the development of products aimed at improving outcomes for students with ASD. NCER may also support projects focused on students with disabilities under their Postsecondary and Adult Education research topic, though no studies focused on ASD have been funded to date under these programs.
Office of Special Education and Rehabilitative Services (OSERS)
The Office of Special Education and Rehabilitative Services (OSERS) supports programs to assist states and school districts in serving children and youth with disabilities, provides for the rehabilitation of youth and adults with disabilities, and supports discretionary grant programs to improve the lives of individuals with disabilities. Through its two main components, the Office of Special Education Programs (OSEP) and the Rehabilitation Services Administration (RSA), OSERS supports a comprehensive array of programs and projects that support individuals with disabilities, including individuals with ASD. OSEP administers the IDEA, and RSA administers the Rehabilitation Act of 1973, as amended by the WIOA. In addition, from 2020 through 2022, in ground-breaking work, ED’s OSERS and Office of General Counsel partnered with CDC’s ADDM program to create a data agreement template under IDEA that permits limited data sharing. This template has been used by CDC’s ADDM sites to obtain critical IDEA data that has helped provide improved data on children with ASD.
The Office of Special Education Programs (OSEP) is responsible for overseeing the administration of the IDEA to assist eligible children and youth with disabilities, including those with ASD. OSEP provides funding to state lead agencies to make available early intervention services to infants and toddlers with disabilities and their families under the IDEA, Part C. OSEP also provides funding to state educational agencies, and through them to local educational agencies, to assist in making a free appropriate public education available to children with disabilities ages 3 through 21 under the IDEA, Part B. Through these formula grants, children with ASD are served as part of all children with disabilities. Autism is one of 13 disabilities that is included in the IDEA, Part B’s definition of "child with a disability" for children ages 3 through 21 in 20 U.S.C. § 1401(3). Autism may be considered a diagnosed condition making children eligible under IDEA, Part C.
During this Administration, there have been significant increases in funding for programs serving students with disabilities, including those with ASD. There has been a $1.26 billion (9.7%) increase in IDEA, Part B state grants, a $58 million (12%) increase in IDEA, Part C state grants for infants and toddlers with disabilities, and a $22 million (5.6%) increase in IDEA state preschool grants.
On March 11, 2021, the American Rescue Plan Act of 2021 (Public Law 117-2) was signed into law. Of the $130 billion that was allocated to the Department, the following amounts were earmarked for IDEA grant awards as supplemental FY 2021 funds: IDEA, Part B - $2.5 billion; IDEA, Part B Preschool - $200 million; and IDEA, Part C - $250 million. All of these funds could be used for children with disabilities, including those with ASD.
In November 2023, HHS and ED announced the release an HHS-ED Policy Statement on Inclusion of Children with Disabilities in Early Childhood Programs. Consistent with a directive to both agencies in Executive Order 14095 on Increasing Access to High-Quality Care and Supporting Caregivers, the statement reiterates expectations for inclusive early childhood settings and updates recommendations for state and local agencies that implement IDEA programs, Head Start, child care, home visiting, preschool, and public schools to increase inclusive early learning opportunities for all children. The statement also includes evidence-based models, exemplars of inclusion, and resources to support high-quality individualized programming and inclusion of children with disabilities in early childhood programs.
OSEP also provides funds through the IDEA’s Part D discretionary grants to benefit children with disabilities, including some grants that have a focus on improving services for children with ASD. While these grants are not specifically in place to implement the Autism CARES Act of 2019, they are funded under IDEA to improve outcomes for infants, toddlers, children, and youth with disabilities.
OSEP currently funds 22 grants that prepare master’s level personnel (e.g., early interventionists, special educators, and related services providers) to serve children with disabilities, with some focus on children with ASD, or doctoral level personnel to conduct research and prepare personnel to teach and support children with disabilities, with some focus on ASD. In FY 2023, OSEP’s personnel preparation program received a $25 million funding increase. These funds were used to increase the number of training grants that were awarded by OSEP in FY 2023. While these funds cannot be disaggregated from the total funding for the training grants, it is likely that some additional ASD training grants were funded.
OSEP also funds projects that generate products and services that are relevant to children with ASD, even though not all of them focus specifically on children with ASD. Some examples are listed below.
- The Early Childhood Technical Assistance Center supports states in implementing Part C and Part B, Section 619, of the IDEA. The Center has a number of resources for state staff on ASD.
- The Center on Positive Behavioral Interventions and Supports provides schools, districts, and state educational agencies with capacity-building information and technical assistance for identifying, adapting, and sustaining effective school-wide disciplinary practices and provides resources on how to prevent and address challenging behaviors, including behaviors related to ASD.
- The National Center for Pyramid Model Implementation provides states with the technical assistance and training to establish the systems and policies needed to adopt and sustain implementation of the Pyramid Model, a framework of evidence-based practices to promote the social, emotional, and behavioral outcomes of young children from birth to age 5; address disparities in discipline practices; promote family engagement; use data for decision-making; and foster inclusion of children with or at risk for developmental delays and disabilities, including children with ASD.
- The State Personnel Development Grants program authorizes competitive grants to state educational agencies to provide in-service professional development to personnel serving children with disabilities, including children with ASD.
- The IRIS Center develops evidence-based professional development and college coursework instructional modules that have addressed aspects of ASD.
- Autism Focused Intervention Resources and Modules (AFIRM) are professional development modules that address instructional and behavioral interventions for young children with ASD. The AFIRM modules are designed to help practitioners learn the step-by-step process of planning for, using, and monitoring evidence-based practices of children with ASD from birth to 22 years of age.
- The National Technical Assistance Center on Transition assists state educational agencies and VR agencies to implement evidence-based and promising practices ensuring students with disabilities, including those with ASD, graduate prepared for success in postsecondary education and employment. The Center has specific resources on secondary transition for students with ASD.
In addition, OSEP funds training and information for families of children with disabilities, including children with ASD. These parent centers, comprised of Parent Training and Information Centers (PTIs) and Community Parent Resource Centers (CPRCs), provide a variety of services, including one-to-one support and assistance, workshops, publications, and resource-rich websites. The Centers help families to:
- Better understand their children’s disabilities and educational, developmental, and transitional needs;
- Communicate more effectively with special education, early intervention, and related services professionals;
- Understand their rights and responsibilities under IDEA; and
- Connect with other local, state, and national resources that assist children with disabilities.
The Center for Parent Information and Resources (CPIR) houses materials for PTIs and CPRCs to use with families. One of CPIR’s resources is the Autism Navigator, which provides information on autism screening, diagnosis, and interventions for young children. CPIR also has an interrelated series of parent guides on youth transition to adult life. While not specific to youth with autism, the series tackles how to develop independent decision-making in youth with disabilities as they and their parents navigate the age of majority and legal adulthood.
The Rehabilitation Services Administration (RSA) is responsible for overseeing the administration of the Rehabilitation Act of 1973, as amended by Title IV of the WIOA, to assist individuals with disabilities, including those individuals with the most significant disabilities, to achieve competitive integrated employment.
RSA funds state VR agencies under Titles I, III, and VI of the Rehabilitation Act to assist VR agencies in providing training and services to individuals with disabilities, including individuals with ASD. RSA also assists states to provide supported employment services to individuals with the most significant disabilities, including the provision of ongoing support services, to enable them to succeed in competitive integrated employment.
Under WIOA, there is a heightened emphasis on serving students and youth with disabilities. The Rehabilitation Act authorizes the provision of pre-employment transition services to students with disabilities, the provision of extended services to youth with the most significant disabilities seeking supported employment outcomes, and sets requirements under Section 511 of the Rehabilitation Act for youth with disabilities seeking or employed in subminimum wage employment to ensure an informed choice regarding opportunities for competitive integrated employment.
Additionally, under Title I of the Rehabilitation Act, RSA funds discretionary grants for the American Indian vocational Rehabilitation Services program to provide services to American Indians with disabilities who live on or near reservations.
Individuals with ASD, including students and youth with ASD, are served through all of these programs. RSA awards discretionary grants, including a national PTI and seven state/regional PTIs to support families of students and youth with disabilities, including those with ASD.
ED-funded projects and agency activities address the following areas of the IACC Strategic Plan: Question 1 (Screening and Diagnosis), Question 4 (Interventions), Question 5 (Services and Supports), Question 6 (Lifespan), and Question 7 (Infrastructure and Prevalence). Within ED’s IES, NCSER continues to encourage a broad range of research on ASD through its field-initiated research competition. This research includes the development and testing of innovative interventions (including programs, policies, and practices) intended to improve the developmental and educational outcomes for students identified with or at risk for ASD from birth through postsecondary education. It also includes support for evaluating new or widely used interventions for efficacy and effectiveness. The grants funded are those rated highly for their research rigor and significance to the field by peer-reviewers, and as evidenced by the projects reported elsewhere in this document, are often relevant to the priorities of the Strategic Plan developed by the IACC. ED is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Table 13: ED funding for ASD activities
| ED Funding for ASD Activities: FY 2019 – FY 2022* | |||||
|---|---|---|---|---|---|
| Fiscal Year | IES** | OSERS*** | TOTAL | ||
| 84.325D | 84.325K | 84.325H | |||
Fiscal Year2019 |
IES*$9,836,498 |
84.325D$12,458,272 |
84.325K$12,326,459 |
84.325H$2,578,041 |
TOTAL$37,199,270 |
Fiscal Year2020 |
IES*$23,668,371 |
84.325D$13,214,836 |
84.325K$16,849,403 |
84.325H$2,574,092 |
TOTAL$56,306,702 |
Fiscal Year2021 |
IES*$25,624,037 |
84.325D$19,040,224 |
84.325K$18,391,928 |
84.325H$2,574,758 |
TOTAL$65,630,947 |
Fiscal Year2022 |
IES*$23,725,135 |
84.325D$25,035,512 |
84.325K$16,349,409 |
84.325H$2,574,078 |
TOTAL$67,684,135 |
Fiscal YearTotal |
IES*$82,854,042 |
84.325D$69,748,844 |
84.325K$63,917,199 |
84.325H$10,300,969 |
TOTAL$143,967,012 |
Data for FY 2023 was not available at the time this report was written.
* While funding under Parts B and C of the IDEA is not listed here, the IDEA funds services for infants, toddlers, children, and youth with disabilities, including those with ASD.
** IES projects with a focus or partial focus on children/youth with autism are included.
*** Funding is provided for the following OSERS Personnel Preparation programs:
- 84.325D: Preparation of Special Education, Early Intervention, and Related Services Leadership Personnel
- 84.325K: Preparation of Early Intervention and Special Education Personnel Serving Children with Disabilities Who Have High-Intensity Needs
- 84.325H: Doctoral Training Consortia Associated with High-Intensity Needs
Department of Housing and Urban Development (HUD)
The Department of Housing and Urban Development (HUD) works to strengthen the housing market in order to bolster the economy and protect consumers, meet the need for quality affordable rental homes, utilize housing as a platform for improving quality of life, and build inclusive and sustainable communities free from discrimination. HUD does not have programs that target specific disabilities, such as housing specifically for people with autism, or programs to specifically implement the Autism CARES Act of 2019. However, HUD-funded programs and activities may directly serve, as well as broadly affect, the well-being of individuals with disabilities, including those with autism and their families.
Section 504 of the Rehabilitation Act of 1973 (29 U.S.C. § 794) prohibits discrimination on the basis of disability in federally assisted programs or activities. Section 504 provisions apply to recipients of HUD financial assistance, including the Community Development Block Grant, public housing, assisted multifamily housing, and the housing choice voucher programs. HUD's regulations for Section 504 that apply to federally assisted programs or activities are found in the Code of Federal Regulations at 24 CFR Part 8; regulations that govern Section 504 in programs conducted by HUD are found in 24 CFR Part 9.
In April 2023, HUD published an Advance Notice of Proposed Rulemaking in the Federal Register seeking the public’s input on potential changes to its regulation implementing Section 504 for recipients of HUD federal financial assistance. The Department is collecting information on what it should consider relating to recipients’ obligations, including how to account for advances in accessible design, the use of websites and other technologies, and auxiliary aids and services including assistive technologies. In addition, HUD is considering whether to adopt an updated federal accessibility standard for purposes of compliance with HUD’s Section 504 regulation.
The HUD Section 811 Supportive Housing for Persons with Disabilities program provides funding to develop and subsidize rental housing with the availability of supportive services for very low- and extremely low-income adults with disabilities.
The program supports two major types of assistance: 1) capital grants and project-based rental assistance for nonprofit developers to build, rehabilitate, or acquire small group homes or scatter site housing units with the availability of supportive services for very low-income persons with disabilities and 2) project-based rental assistance for state housing agencies in partnership with state health and human services/Medicaid agencies to provide housing for extremely low-income persons with disabilities with access to appropriate supportive services.
Program eligibility differs by project type. For projects funded by capital advances and supported by project rental assistance contracts, households must be very low-income (within 50% of the median income for the area) with at least one adult member with a disability. For projects funded with project rental assistance, households must be extremely low-income (within 30% of the median income for the area) with at least one adult member with a disability. States may also establish additional eligibility requirements for this program.
In August 2020, HUD awarded over $74 million in grants to 12 state housing agencies to support affordable rental housing for extremely low-income persons with disabilities. The awards will support up to five years of rental assistance for approximately 2,400 units of housing in buildings participating in project rental assistance through the Section 811 program. HUD also awarded $54.7 million in capital advance and project rental assistance grants to 15 community organizations through the Section 811 program. The grants were awarded to organizations who will create permanent supportive housing models that will be at the forefront of design, service delivery, and efficient use of federal resources. Awardees must promote long-term housing security and facilitate community integration of persons with disabilities. In 2020, HUD issued an eviction moratorium and offered additional funds to properties receiving project-based rental assistance under the Section 811 program, as part of the CARES (Coronavirus Aid, Relief, and Economic Security) Act of 2020.
The program is authorized by Section 811 of the National Affordable Housing Act of 1990 (Public Law 101-625), as amended by the Housing and Community Development Act of 1992 (Public Law 102-550), the Rescission Act (Public Law 104-19), the American Homeownership and Opportunity Act of 2000 (Public Law 106-569), and the Frank Melville Supportive Housing Act of 2010 (Public Law 111–374). Program regulations are in 24 CFR Part 891.
Mainstream Vouchers assist very low-income adults with disabilities with tenant-based rental assistance. The program is administered by local public housing agencies and enables participants to rent housing in the private market. Public housing agencies that administer these vouchers are encouraged to establish formal partnerships with multiple health and human service agencies or organizations with a demonstrated capacity to coordinate voluntary services and supports to enable individuals to live independently in the community. Since 2018, HUD has awarded over $500 million in funding to public housing authorities (PHAs) to support 50,000 new Mainstream Vouchers. Under the authority of the CARES Act, HUD allocated nearly $77 million for Mainstream Vouchers in May 2020 and another $87 million in November 2020. In June 2022, HUD announced the availability of $40 million in carryover funding for additional Mainstream Vouchers to support community living for persons with disabilities, and later in July 2022, HUD awarded over $36 million in Mainstream Vouchers and fees to support community living for people with disabilities. In January 2023, HUD announced the award of $24.7 million to 98 local PHAs across the country to provide permanent affordable housing to non-elderly persons with disabilities, which will allow these PHAs to house up to 2,210 additional families and further support community integration for persons with disabilities.
The statutory authority for the Mainstream Voucher Program is the Cranston-Gonzalez National Affordable Housing Act, 42 U.S.C. § 8013 (Public Law 101-625), as amended by the Frank Melville Supportive Housing Act of 2010 (Public Law 111-374), the Consolidated Appropriations Act, 2018 (Public Law 115-141), and the Consolidated Appropriations Act, 2019 (Public Law 116-6).
Since 1997, housing choice vouchers have been awarded under different special purpose voucher program types to serve very low-income non-elderly adults with disabilities (NED). NED Vouchers enable non-elderly disabled families to lease affordable private housing of their choice and assist persons with disabilities who often face difficulties in locating suitable and accessible housing in the private market. Program regulations are found in 24 CFR Part 892.
The Fair Housing Act protects people from discrimination when they are renting or buying a home, getting a mortgage, seeking housing assistance, or engaging in other housing-related activities. Additional protections apply to federally assisted housing. The Fair Housing Act prohibits discrimination in housing because of race, color, national origin, religion, sex (including gender identity and sexual orientation), familial status, and disability.
In July 2021, HUD announced that it made $19.4 million available through HUD’s Fair Housing Initiatives Program (FHIP) to fair housing organizations to conduct activities that address discriminatory housing practices related to the COVID-19 pandemic. The funds, which were provided through the American Rescue Plan Act of 2021, allow private fair housing enforcement organizations to respond to fair housing inquires and complaints, conduct fair housing testing, and implement education and outreach activities related to the COVID-19 pandemic. The funds are also being used to address fair housing issues affecting individuals and families experiencing housing instability, including those who may face displacement due to discriminatory evictions and foreclosures.
In September 2021, HUD awarded $47.4 million to fair housing organizations across the country under its FHIP. The grants support the efforts of 120 state and local fair housing organizations working to address and prevent violations of the Fair Housing Act and helping to end discrimination in housing.
In June 2022, HUD allocated over $30 million in funding for state and local fair housing enforcement agencies across the country under the Department's Fair Housing Assistance Program. HUD also issued guidance on the investigation of housing discrimination complaints that allege discrimination based on a housing provider’s use of criminal records in tenant screening that specifically discusses how such practices can result in disability discrimination. More than $28 million was made available to fair housing organizations across the nation working to fight housing discrimination under FHIP.
In March 2023, HUD awarded $54 million to 182 fair housing organizations across the country under FHIP. The grants will provide $28.2 million to support the efforts of national, state, and local fair housing entities working to address violations of the Fair Housing Act and helping to end discrimination in housing. In addition, HUD provided over $26 million in funding to its second- and third-year Private Enforcement Initiative grantees to continue fair housing enforcement efforts nationwide.
In addition to barring housing discrimination, the Fair Housing Act requires HUD and its funding recipients, such as local communities receiving HUD funds, to take affirmative steps to remedy fair housing issues such as segregated neighborhoods, lack of housing choice for protected class groups (including persons with disabilities), and unequal access to housing-related opportunities. In 2023, HUD issued a major Proposed Rule to restore the Affirmatively Furthering Fair Housing mandate. As stated by HUD, the rule "aims to remedy the effects of the long history of discrimination in housing, will help to foster opportunity in communities across the country where every resident can thrive," and "spur HUD program participants to take action in order to ensure members of protected classes have equitable access to affordable housing opportunities." Under the proposed rule, HUD grant recipients would be required to prepare an Equity Plan, to "be developed following robust community engagement, would contain their analysis of fair housing issues confronting their communities, goals, and strategies to remedy those issues in concrete ways, and a description of community engagement." Additionally, HUD is committed to providing communities that receive HUD funding with the technical support they need to meet their long-standing fair housing obligations.
While HUD does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by HUD, including through the programs described above, are available to individuals with disabilities, including those on the autism spectrum and their families. These programs are intended to improve well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. HUD activities are also relevant to Question 6 (Lifespan) of the IACC Strategic Plan. HUD is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Department of Justice (DOJ)
The U.S. Department of Justice (DOJ) ensures fair and impartial administration of justice for all Americans. DOJ-funded research and activities broadly impact the well-being of individuals with disabilities, including those with ASD, and their families.
Civil Rights Division
Within DOJ, the Civil Rights Division works to uphold the civil and constitutional rights of people with disabilities, including people with ASD and other developmental disabilities. The Division coordinates the implementation and enforcement of Section 504 of the Rehabilitation Act and Title II of the Americans with Disabilities Act (ADA) across the federal government. Section 504 of the Rehabilitation Act states that "no qualified individual with a disability in the United States shall be excluded from, denied the benefits of, or be subjected to discrimination under" any program or activity that either receives federal financial assistance or is conducted by any Executive agency or the U.S. Postal Service. Title II of the ADA requires that state and local governments give people with disabilities an equal opportunity to benefit from all of their programs, services, and activities (e.g., public education, employment, transportation, recreation, health care, social services, courts, voting, and town meetings). Title II covers all activities of state and local governments regardless of the government entity's size or receipt of federal funding.
The Disability Rights Section (DRS) of DOJ administers and enforces the ADA to achieve equal opportunity for people with disabilities in the United States. DRS has addressed the unnecessary segregation of people with intellectual and developmental disabilities and expanded opportunities for people with intellectual and developmental disabilities to work in competitive integrated employment. DRS has also addressed alleged discrimination by private schools and childcare centers against students with ASD on the basis of their disability. The Section also coordinates the implementation and enforcement of Section 504 of the Rehabilitation Act and Title II of the ADA across the federal government. Key concepts that are common to the Department’s Section 504 and ADA regulations include reasonable modifications, program accessibility, and effective communication.
The Educational Opportunities Section enforces anti-discrimination statutes, including the ADA, Section 504 of the Rehabilitation Act, the Equal Educational Opportunities Act, and Title VI of the Civil Rights Act, in elementary and secondary schools and institutions of higher education. The Section also upholds rights under the 14th Amendment to the U.S. Constitution in educational settings.
- DOJ is currently challenging the State of Georgia’s operation of the Georgia Network for Educational and Therapeutic Supports (GNETS) Program, a statewide network of segregated special education programs, on the ground that the state’s operation of the program discriminates against students with disabilities. Approximately 4,000 students are enrolled in segregated GNETS facilities across the state, including students with autism.
- DOJ has recently entered into numerous agreements with school districts to address the discriminatory use of seclusion and restraint against students with disabilities, including students with autism. DOJ has also entered into several agreements with school districts to ensure that English learner students who have disabilities, including students with autism, receive the educational services to which they are entitled and that school districts effectively communicate with any of those students’ parents who are limited-English proficient.
The Special Litigation Section of DOJ enforces Title II of the ADA, the Civil Rights of Institutionalized Persons Act, and 34 U.S.C. § 12601 of the Violent Crime Control and Law Enforcement Act of 1994. The Section’s work has addressed conditions at health care facilities for individuals with disabilities, the rights of individuals with disabilities to live in their communities and not facilities, and the appropriate diversion of individuals with disabilities from the criminal justice system.
Office of Justice Programs (OJP)
The Office of Justice Programs (OJP) within DOJ provides grant funding, training, research, and statistics to the criminal justice community and their partnering agencies. The OJP focuses on equipping and strengthening communities, justice systems, and other sectors through the dissemination of innovative and best practices, research, and statistics; grant funding and technical assistance; and fostering relationships.
The Bureau of Justice Assistance (BJA) is one of several divisions located within the OJP. BJA’s mission is to assist states, tribes, and local governments to reduce and prevent crime. BJA provides strategies and best practice approaches to promote a fair and safe criminal justice system. Communities can apply to receive grant funding, training, and technical assistance to support law enforcement, courts, correctional agencies, treatment providers, reentry practitioners, justice information technologists, and community-based partnerships to address the challenges unique to every community.
The five primary strategic focus areas at BJA are building trust and ensuring an effective criminal justice system, reducing recidivism and unnecessary contact with the criminal justice system, utilization of confidence-based strategies, increasing program effectiveness, and ensuring organizational excellence. Through this lens, BJA strives to improve and enhance criminal justice system responses to people with mental health disorders and co-occurring mental health and substance use disorders and people with intellectual and developmental disabilities such as autism.
The Justice and Mental Health Collaboration Program (JMHCP), authorized through the Justice and Mental Health Collaboration Reauthorization Act of 2022 (Public Law 117-323), supports innovative cross-system collaboration for individuals with mental illnesses or co-occurring mental health and substance abuse disorders who come into contact with the justice system. JMHCP provides grant programming, resources, and free training and technical assistance through BJA’s cooperative agreement recipient partner, the Council of State Governments Justice Center, and at JMHCP.org.
In 2022, JMHCP released the Field Notes brief Improving Outcomes for People in Contact with the Criminal Justice System Who Have Intellectual or Developmental Disabilities. The brief describes how people with intellectual and developmental disabilities can become involved in the criminal justice system and existing misconceptions within the criminal justice system regarding abilities and needs. However, there are ways to help improve outcomes for people with intellectual and developmental disabilities and reduce their chances of re-encountering the criminal justice system. This brief offers important steps that criminal justice administrators can take to better identify and respond to the needs of people with intellectual and developmental disabilities.
In 2023, JMHCP released the brief Supporting Improved Responses to People with Intellectual and Developmental Disabilities. Through a partnership with The Arc’s National Center on Criminal Justice and Disability and the Council of State Governments Justice Center, four Justice and Mental Health Collaboration grant programs received technical assistance and support to improve their responses to people with intellectual and developmental disabilities. Based on this assistance, four overarching themes emerged that can be used to guide other programs in their efforts to enhance responses to this population. The brief highlights those themes and gives an overview of each grantee’s program, including the work they have done with the help of this technical assistance.
Academic Training to Inform Police Responses is another BJA initiative that is authorized and funded through the Edward Byrne Justice Assistance Grant Program, through a carve out to support law enforcement training. Under this initiative, the Collaborative Crisis Response and Intervention Training Program supports best practice responses that include specific training on response for people with intellectual and developmental disabilities, inclusive of people with ASD.
The Collaborative Crisis Response Training Program (site-based grant program) funds the implementation of transdisciplinary crisis response training to educate, train, and prepare law enforcement and corrections officers so that they are equipped to appropriately interact with people who have behavioral health conditions (including mental health and substance use) and intellectual and developmental disabilities while completing their job responsibilities. The program supports states and local law enforcement and correctional entities to plan and implement training, engage in organizational planning to deploy trained officers in times of crisis, and sustain a best practice crisis response program. This program supports site-based awards, training, and technical assistance.
Under the Academic Training Initiative, several products and webinars have been developed that provide information and best practices related to police responses to people with intellectual and developmental disabilities. The Bureau of Justice Assistance Style Guide for Using the Sequential Intercept Model: Behavioral Health and Intellectual and Developmental Disability Considerations was published in August 2021; this document contains guidelines for content related to criminal justice and behavioral health and intellectual and developmental disabilities, including concepts, terminology, and definitions. Mental Health Conditions & Developmental Disabilities: Why Know the Difference? is a two-page resource published in April 2022 that describes mental health conditions and developmental disabilities, common behaviors and characteristics, and the differences between mental health conditions and developmental disabilities. Also published in April 2022, Developmental Disabilities: What Law Enforcement Officers Need to Know is a two-page resource that provides examples of law enforcement encounters with people with developmental disabilities, discusses how understanding more about disabilities leads to safe and effective interactions, and includes possible behaviors of people with developmental disabilities and recommended responses. Law Enforcement Response to People with Developmental Disabilities: Steps for Deflection or Pre-Arrest Diversion is a multi-page guide published in February 2023 that provides insights into the developmental disability community, offers suggestions for successful interactions with people with developmental disabilities, and outlines options for safe and effective deflection and pre-arrest diversion when people with developmental disabilities encounter law enforcement and may be experiencing a crisis or are otherwise in need of services.
The Academic Training Initiative hosted the webinar Policing and People with Developmental Disabilities: Emerging Issues in the Field on April 28, 2022, that provided an overview of police interactions with people with developmental disabilities from the perspectives of law enforcement and a person with a developmental disability, including emerging issues and practical tips officers can use to respond effectively to this population. On December 8, 2022, the Academic Training Initiative hosted the webinar Integrating Behavioral Health Peer Support Specialists into Crisis Response that provided an overview of the roles of behavioral health peer support specialists across the criminal justice system, discussed the newer role of peer support specialists in crisis response, provided examples of how peer support specialists are trained and embedded in teams of professionals tasked with responding to crisis calls in the community, and discussed how people with intellectual and developmental disabilities might be integrated into similar peer support roles to enhance crisis responses to people with intellectual and developmental disabilities.
The Crisis Response and Intervention Training (CRIT) is a 40-hour training program designed to prepare police officers in their response to people experiencing crises related to behavioral health conditions (including mental health conditions and substance use disorders) and intellectual and developmental disabilities. This training is based upon the Memphis Model of Crisis Intervention Team training and is designed to complement the development and delivery of crisis response programs planned by law enforcement agencies, behavioral health services providers, and disability service providers in the community. In December 2022, the Academic Training Initiative published the CRIT curriculum as part of the CRIT Toolkit, which includes resources needed to support the coordination and delivery of the training in a law enforcement agency.
Kevin and Avonte’s Law (H.R. 4221 and S. 2070) was named in honor of two boys with autism who wandered from safety and tragically lost their lives. This site-based grant program, along with training and technical assistance, supports local jurisdictions’ efforts to reduce the number of deaths and injuries of individuals with forms of dementia such as Alzheimer’s disease or developmental disabilities such as autism who, due to their condition, wander from safe environments. Training and technical assistance is available through the Home Safe project to support site-based grantees and the field. The Home Safe Library of Resources is a searchable compilation of webinars, workshops, tools, articles, publications, and other resources to support local jurisdictions’ efforts to reduce the number of deaths and injuries of individuals with forms of dementia such as Alzheimer’s disease, or developmental disabilities such as autism who, due to their condition, wander from safe environments.
While DOJ does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by DOJ are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. DOJ activities are also relevant to Question 5 (Services and Supports) and Question 6 (Lifespan) of the IACC Strategic Plan. DOJ is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Department of Labor (DOL)
The U.S. Department of Labor (DOL) works to foster full access to gainful employment opportunities for all Americans, including youth and adults on the autism spectrum or with other disabilities. DOL also seeks to advance career pathways for youth and adults through its support for workforce development and job training programs, including apprenticeships. The Office of Disability Employment Policy (ODEP) within DOL runs autism-focused projects and related efforts, but these activities are not specifically in place to implement the Autism CARES Act of 2019.
ODEP began its project on Research Support Services for Employment of Young Adults on the Autism Spectrum (REYAAS) in August 2021. ODEP developed the REYAAS project after a request from congressional appropriations to expand research on access to employment and transition from school to work for autistic young adults, defined as ages 16 to 28. The REYAAS project has received approximately $2.9 million in funding to date under a contract with Mathematica. ODEP staff provide oversight and review of work conducted by Mathematical staff. A technical working group of key subject matter experts in autism, employment, and career development issues has also advised the project’s work.
The REYAAS project conducted an extensive review of the research literature for evidence-based program models, strategies, and practices to support employment access. This review analyzed peer-reviewed literature published in recent years to identify findings, themes, and knowledge gaps. In 2022, the REYAAS project released two resources that highlight promising approaches and practices to support employment and career access:
- Programs, Models, and Strategies to Support Employment Outcomes of Young Adults on the Autism Spectrum
- Evidence on the Effectiveness of Programs, Models, and Strategies to Support Employment Outcomes of Young Adults on the Autism Spectrum
The REYAAS project also conducted extensive listening sessions with groups that share an interest in supporting employment and career pathways for autistic youth and young adults. These groups included youth and young adults on the autism spectrum (multiple sessions), employers, direct service providers, educators, researchers, advocates, and policymakers. A total of 147 participants, including 97 autistic youth and young adults, participated in the listening sessions. Their insights, thoughts, and perspectives shaped the REYAAS project’s 2022 resource on Barriers and Facilitators to Employment and Careers for Young Adults on the Autism Spectrum.
More recently, the REYAAS project analyzed use of VR services by youth and young adults on the autism spectrum. This analysis focused on use of services provided by state VR agencies and employment outcomes for autistic youth and young adults from program year (PY) 2017-2020. It resulted in a 2023 REYAAS resource titled Characteristics, Service Use, and Employment Outcomes of Young Adults on the Autism Spectrum Who Engaged with Vocational Rehabilitation Services from 2017 to 2020.
Launched in 2019, the Center for Advancing Policy on Employment for Youth (CAPE-Youth) helps address barriers that youth and young adults with disabilities may face. CAPE-Youth focuses on the transition from youth systems into adulthood and barriers that can result in lower employment outcomes, educational attainment, and community participation. CAPE-Youth works to improve employment outcomes by helping states build capacity in their youth service delivery and workforce systems and conducts research, develops partnerships, and shares best and promising practices. The Center also helps states identify new ways to expand career pathways, work-based learning, strategic partnerships, and coordination of systems. The Guideposts for Success: Framework for the Future drives the work of CAPE-Youth by outlining the five key domains for programs and services: preparing for careers, school life, engagement with families, youth development and leadership, and connecting activities.
ODEP launched the Advancing State Policy Integration for Recovery and Employment (ASPIRE) initiative in 2020. ASPIRE seeks to support and expand access to competitive, integrated employment for people with mental health conditions. It assists seven states in integrating their policies, programs, and funding systems to expand evidence-based mental health services for people with mental health conditions. ASPIRE emphasizes the use of best and promising practices, such as the Individual Placement and Support model of supported employment.
Since 2020, ODEP’s Partnership on Employment & Accessible Technology (PEAT) has discussed how to help drive support for neurodiversity in technology workplaces and tap skills and talents. The PEAT project has released podcasts on its website that examine this focus in depth. These podcasts for neurodiversity in the space of technology fields include:
- Neurodiversity & Workplace Technology
- The Future of Autism Hiring Programs
- Building Neurodiverse Talent Pools
In 2021, ODEP’s Employer Assistance and Resource Network on Disability Inclusion (EARN) released its updated online guide for Neurodiversity in the Workplace. This guide from EARN highlights core advantages for employers and workforces in industry and government to recruit, hire, retain, and advance workers who are neurodivergent, including autistic people. It also discusses approaches to help support management, peer training, and mentoring for neurodivergent workers and describes examples of companies and agencies with focused hiring programs. Released in 2022, EARN’s webinar on Hiring and Supporting Neurodivergent Workers: Strategies for Success and its companion learning guide examine these promising practices. Likewise, EARN’s Checklist for Organizational Success discusses key steps for employers to advance efforts to foster full support for neurodiversity in workplace inclusion.
ODEP initiated the Partnership on Inclusive Apprenticeship (PIA) project in 2021 to bolster and enhance access to career pathways in high-growth, high-demand fields in the economy. The PIA project has released resources on how to design and foster access to inclusive apprenticeships that support employers, intermediaries, and apprentices and career seekers. PIA also hosts the Apprenticeship for All Podcast series. A recent episode of this series discussed Strengths-Based Practices to Support Neurodiversity at Work with Dr. Scott Michael Robertson, a senior policy advisor at ODEP and an autistic adult.
The ODEP-funded Job Accommodation Network (JAN) provides free, expert, and confidential assistance and guidance for job seekers and workers with disabilities, employers, and all others. JAN’s website offers a resource on work accommodations and supports for people on the autism spectrum and a resource on interviewing tips for autistic job applicants. During National Autism Month 2023, JAN hosted a webinar on Accommodation Solutions for Neurodivergent Workers for its training series, and in August 2023, it launched a new accommodation webpage on Neurodiversity. Featuring resource links and real-life examples, the page describes common workplace challenges faced by neurodivergent employees and accommodation ideas to help them perform their work and maximize their talents and skills.
Managed jointly by ODEP and the DoD, the Workforce Recruitment Program (WRP) is a recruitment and referral program that connects employers from the federal and private sectors with college students and recent graduates with disabilities, including people who are neurodivergent, for internships and permanent jobs. WRP candidates can apply annually through their school campuses and take part in elective informational interviews with federal workers who serve as volunteer recruiters. The Office of Personnel Management recognizes WRP as a model strategy in its guidance to federal agencies regarding the recruitment and hiring of people with disabilities. Since the program’s expansion in 1995, thousands of students and recent graduates have received temporary and permanent opportunities for gainful employment through the WRP.
ODEP’s State Exchange on Employment & Disability (SEED) initiative is a unique state-federal collaboration that supports state and local governments in developing and implementing disability-inclusive policies and best practices that lead to increased employment opportunities for people with disabilities, including those on the autism spectrum. SEED supports partnerships and collaborations with 19 state and local intermediary organizations that reach more than 7,000 legislators, 50 governors, 50 lieutenant governors, 1,400 mayors, and 3,000 county governments. By leveraging its intermediary partners, the SEED collaborative supports states’ needs through testimony and expertise; state priority mapping, data collection, and policy analysis; and policy development and implementation support. State policy options range from examining state disability employment policies and expanding transportation options for job seekers with disabilities to providing incentives for the private sector to employ people with disabilities and fostering youth transition policies.
In addition to policy development work with states and federal agencies, ODEP shares key resources and information on employment topics through its website. ODEP’s autism webpage provides resources and information for employers, job seekers, transition age youth on the autism spectrum, service providers, and policymakers. Additionally, ODEP’s website offers topic resource pages on a variety of issues, including mental health and health care.
DOL’s Employee Benefits Security Administration (EBSA) enforces Title I of the Employee Retirement Income Security Act (ERISA) of 1974, including requirements of the Mental Health Parity and Addiction Equity Act (MHPAEA) of 2008 with respect to two and a half million private employment-based group health plans, which cover approximately 133 million participants and beneficiaries. MHPAEA generally provides that financial requirements such as coinsurance and copays and treatment limitations such as visit limits imposed on mental health or substance use disorder benefits cannot be more restrictive than the predominant financial requirements and treatment limitations that apply to substantially all medical/surgical benefits in a classification. In addition, MHPAEA prohibits separate treatment limitations that apply only to mental health/substance use disorder benefits. EBSA has issued guidance to emphasize that plans and issuers must ensure that treatment limitations on benefits for ASD do not violate the requirements of MHPAEA, including benefits for ABA therapy. EBSA also recently proposed a rule to update the requirements based on EBSA’s experience enforcing MHPAEA and to further MHPAEA’s fundamental goals. This proposed rule would, if finalized, clarify that ASD is a mental health condition for purposes of the protections of MHPAEA.
EBSA is committed to ensuring that participants and beneficiaries on the autism spectrum in ERISA-covered plans can access interventions to improve health and well-being. Vigorous enforcement of MHPAEA has been one of the agency’s top enforcement priorities, with EBSA working with health insurance issuers and other service providers to group health plans to obtain widespread correction of violations affecting multiple group health plans. In a recent enforcement action, EBSA investigated exclusions of coverage for ABA therapy by service providers to self-insured plans. As a result of these investigations, several large service providers have made changes to provide coverage of ABA therapy for their self-insured plan clients, affecting close to 1.5 million participants.
While DOL does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by DOL are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. DOL activities are also relevant to Question 5 (Services and Supports) and Question 6 (Lifespan) of the IACC Strategic Plan. DOL is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Department of Transportation (DOT)
The U.S. Department of Transportation (DOT) works to ensure transportation that is fast, safe, efficient, accessible, and convenient to improve the quality of life of people in the United States. DOT does not receive funding from the Autism CARES Act of 2019; however, DOT-funded research and activities do broadly impact the well-being of individuals with disabilities, including those on the autism spectrum and their families, and help to ensure access to important supports including disability employment, recreational activities, community living, and respite for family caregivers.
The Coordinating Council on Access and Mobility (CCAM) is a federal interagency council tasked with coordinating human services transportation for transportation disadvantaged populations. DOT’s Federal Transit Administration (FTA) leads the CCAM, on behalf of the Secretary of Transportation, in coordination with 10 other federal departments and agencies. CCAM members include the U.S. Departments of Health and Human Services, Education, Labor, Veterans Affairs, Agriculture, Housing and Urban Development, Interior, and Justice, as well as the SSA and the National Council on Disability. The CCAM’s mission is to improve the availability, accessibility, and efficiency of transportation for people with disabilities, older adults, and individuals of low income. The CCAM convened at DOT on October 27, 2022, and officially adopted the 2023 – 2026 CCAM Strategic Plan, which sets the CCAM’s priorities for the four-year period.
FTA provides financial and technical assistance to local public transit systems, including buses, subways, light rail, commuter rail, trolleys, and ferries. FTA also oversees safety measures and helps develop next-generation technology research. All FTA activities aim to support mobility for all individuals. The exploration, testing, validation, and dissemination of technologies and service modes is driven by a vision of carefree mobility, in which each person can readily meet the travel needs they have. Whether it is easier trip planning and payment or more responsive microtransit systems, FTA is fielding solutions to common mobility challenges and supporting complete trips for all.
One example of this work is the Accessible Transportation Technologies Research Initiative (ATTRI), which is a joint multi-modal, multi-agency initiative, co-led by FTA, the Federal Highway Administration, and Intelligent Transportation Systems Joint Program Office, with support from NIDILRR within HHS/ACL and other federal partners. The ATTRI program developed and implemented transformative applications to improve mobility options for all travelers, particularly those with disabilities. ATTRI research focuses on removing barriers to transportation for people with visual, hearing, cognitive, and mobility disabilities. Technologies and creative service models funded by ATTRI offer all Americans enhanced travel choices and accessibility at levels once only imagined.
FTA additionally funds several national technical assistance centers, each with its mission. Collaboratively, the centers are working to improve mobility for all through the coordination of transportation services. Three of FTA’s technical assistance centers completed autism- and/or developmental disabilities-related transportation activities during FY 2019 – FY 2023, described below.
- National Center for Mobility Management (NCMM)
- National Activities
- In November 2022, NCMM conducted a webinar on Strategies to Address Transportation Challenges for the National Center on Rehabilitation Training Materials, whose audience is professionals working with individuals with autism and other cognitive disabilities.
- NCMM conducted workshops at the 2022 Council for Exceptional Children Convention and the 2022 Division on Career Development and Transition Forum targeted at youth transition professionals working to develop transportation education skills for students with significant disabilities, including cognitive disabilities.
- NCMM published the article Don’t Forget About Transportation in January 2022 to promote NCMM technical assistance supports to the AUCD.
- In 2013, NCMM contributed to a chapter in AUCD’s publication A Collaborative Interagency, Interdisciplinary Approach to Transition from Adolescence to Adulthood. This publication continues to be used by the public as a resource on transportation issues related to transition age youth.
- State and Regional Activities
- NCMM implemented a curriculum for youth transition and workforce development professionals working with individuals with autism in Maryland and focused on building relationships across education, VR, and transportation services to support youth transition.
- NCMM helped build the mobility management network in New Hampshire that includes the participation of ACF and diverse state agencies.
- NCMM facilitates a transportation coordination council for the state of Missouri on which the Missouri Developmental Disabilities (MDD) Council actively participates. The forum provides an opportunity for information exchange and capacity building regarding mobility management and leveraging accessible transportation services for individuals with intellectual and developmental disabilities served by the MDD Council.
- In Illinois, at the request of the Department of Disability and Human Development at the University of Illinois Chicago, NCMM provided technical assistance to provide transportation resources for individuals with cognitive disabilities.
- In June 2022, NCMM conducted a workshop to the Indiana VR Counseling Supervisors Circle on transportation supports for individuals with significant disabilities.
- National Aging and Disability Transportation Center (NADTC)
- The 2021 NADTC Trends Report Serving People with Autism on Transportation includes an overview of autism, describes transportation challenges faced by people with autism, and provides tips and promising practices for serving individuals with autism.
- The 2020 NADTC Trends Report Transportation for People with Intellectual and Developmental Disabilities provides an overview of intellectual and developmental disabilities, describes what barriers people with intellectual and developmental disabilities face with regards to transportation, and includes examples of programs with effective strategies to increase transportation accessibility for people with intellectual and developmental disabilities.
- A December 2021 NADTC blog post described how adult changing stations have become common amenities in several states and how they make traveling with a person with a disability more accessible.
- An NADTC blog post published in September 2020 discussed appropriate language when talking about and with people with disabilities.
- NADTC’s Learning Center hosts a collection of educational videos, including Access Matters videos that discuss how accessible transportation improve the lives of older adults and people with disabilities, effective communication for transportation operators to ensure people with disabilities are treated with respect, regulations surrounding service animals on public transportation, and tips for transportation operators in providing various types of assistance for people with and without disabilities.
- NADTC provides direct technical assistance for people looking for transportation for individuals with various disabilities, including autism and other developmental disabilities, as well as programs inquiring of the best way to serve people with disabilities. In FY 2019 – FY 2023, NADTC provided direct technical assistance to meet the transportation needs of seven individuals on the autism spectrum and advised on the process and legality of notifying transportation operators of a passenger with autism or other needs.
- National Rural Transit Assistance Program (RTAP)
- On February 16, 2023, National RTAP conducted a Books in Transit Discussion Group Meeting with Rachel Simon, author of the book Riding the Bus with My Sister. The book is a memoir about the author’s sister who has an intellectual disability and spends her days riding the buses in a Pennsylvania city.
- National RTAP and NADTC held an #AllOnboard4MentalHealth Twitter chat on October 11, 2022. Heather Edmonds and Jane Mahoney of NADTC and Cara Marcus of National RTAP discussed best practices and equitable strategies for serving riders with mental health issues.
- In March 2022, National RTAP provided direct technical assistance to a Tribal member and Veteran with an autistic son who needed transportation and additional social service supports.
- In February 2022, a transit manager asked for training for drivers of passengers with autism. National RTAP provided resources from NADTC, the Massachusetts Center for Developmental Disabilities, and East Carolina University Disability Support Services.
- National Activities
While DOT does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by DOT are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. DOT activities are also relevant to Question 5 (Services and Supports) and Question 6 (Lifespan) of the IACC Strategic Plan. DOT is a member of the IACC and the FIWA and participates in efforts to coordinate autism activities across the federal government.
Department Of Veterans Affairs (VA)
The Department of Veterans Affairs (VA) is committed to serving and honoring America’s veterans by ensuring access to timely, high-quality benefits and services. As part of this commitment, the VA’s Veterans Health Administration delivers health care to the nine million enrolled veterans each year, including veterans with autism or other disabilities, through the largest integrated health care network in the United States, with 1,298 health care facilities. VA offers diagnostic services and treatment within VAs that have commensurate specialists, as well as offers Community Care for all other treatment options. In addition, the Civilian Health and Medical Program of the Department of Veterans Affairs, a health benefits program which provides coverage to the spouse or widow(er) and children of veterans not eligible for TRICARE, allows ABA as a covered health benefit.
While the VA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by the VA are available to individuals with disabilities, including those on the autism spectrum and their families. These services are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. VA activities are relevant to Question 4 (Interventions), Question 5 (Services and Supports), and Question 6 (Lifespan) of the IACC Strategic Plan. The VA is a statutory member of the IACC, a member of the FIWA, and participates in efforts to coordinate autism activities across the federal government.
Environmental Protection Agency (EPA)
The U.S. Environmental Protection Agency (EPA) aims to protect human health and the environment through such activities as the development and enforcement of environmental regulations, the support of grants and laboratories for scientific research, and the publication of materials for public access. EPA works to ensure that all parts of society have access to accurate information sufficient to effectively participate in managing human health and environmental risks. EPA-funded research and activities broadly impact the health and well-being of individuals with disabilities, including those with ASD and their families.
The goal of the Children's Environmental Health and Disease Prevention Research Centers (Children's Centers), an extramural grant program that was jointly funded by EPA and NIEHS, was to understand how environmental factors affect children's health and promote translation of basic research findings into interventions and prevention methods to prevent adverse health outcomes. The 2013 EPA Children's Centers award to the University of California, Davis was funded under EPA's Science to Achieve Results grant program and focused on environmental risk factors for ASD and developmental delays. Specifically, the University of California, Davis center studied the epigenetic mechanisms of toxicant exposure on immune function, developed and applied new biomarkers of autism risk, characterized the potential health effects of environmental exposures and various life stages, and predicted long-term clinical and behavioral consequences. The environmental chemicals that this center examined with regard to ASD included polybrominated diphenyl ethers, perfluorooctanoic acid, perfluorooctanesulfonic acid, and pesticides. Several notable research findings resulted from this project, and Children's Centers researchers identified potential links between air pollution, pesticides, occupational exposures, phthalates, and risks of ASD. This project was funded through FY 2019.
EPA also provides funding to the Agency for Toxic Substances and Disease Registry, under an interagency agreement, to support 10 Pediatric Environmental Health Specialty Units (PEHSUs). PEHSUs provide medical information and advice on environmental conditions, including working with health care professionals, parents, schools and community groups, and others to provide information on protecting children and reproductive-age adults from environmental hazards. PEHSUs offer advice on prevention, diagnosis, management, and treatment of environmentally related health effects in children.
Active research supported by EPA focuses on advancing alternatives to vertebrate animal toxicity testing to assess impacts of chemical exposures on neurodevelopment. Extramural grants funded by EPA that impact the health and well-being of individuals on the autism spectrum include grants on the Multiplexed human BrainSphere Developmental Neurotoxicity Test for Six Key Events of Neural Development (R839505; Johns Hopkins University) and the Integrated blood brain barrier – computational model development to predict doses of concern for compound linked neurotoxicity (RD840027; Purdue University).
In FY 2023, EPA funded an intramural research project titled "Expanding and Improving Alternative Species Methods to Detect and Characterize Developmental Neurotoxicity." This research is intended to reduce uncertainty in the detection and characterization of developmental neurotoxicity using alternatives to vertebrate animal models by increasing biological coverage of neurodevelopmental processes commonly affected in nervous system disorders, including ASD.
While EPA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, EPA-funded research addresses Question 3 (Genetic and Environmental Factors) of the IACC Strategic Plan. EPA is a member of the IACC and the FIWA and participates in efforts to coordinate autism activities across the federal government.
Institute of Museum and Library Services (IMLS)
The mission of the Institute of Museum and Library Services (IMLS) is to advance, support, and empower America’s museums, libraries, and related organizations through grantmaking, research, and policy development. IMLS envisions a nation where individuals and communities have access to museums and libraries to learn from and be inspired by the trusted information, ideas, and stories they contain about our diverse natural and cultural heritage. While IMLS does not receive funding from the Autism CARES Act of 2019, IMLS funds several projects relevant to individuals with autism and other developmental disabilities, including providing funding to increase accessibility and maximize inclusion at museums and libraries throughout the nation and developing services for children on the autism spectrum.
Through its Grants to States Program, IMLS distributes approximately $180 million among the State Library Administrative Agencies (SLAAs) each year. SLAAs are the official agencies charged by law with the extension and development of library services, and they are located in each of the 50 states and the District of Columbia; the Territories (Guam, American Samoa, the Commonwealth of Puerto Rico, the Commonwealth of the Northern Mariana Islands, and the U.S. Virgin Islands); and the Freely Associated States (Federated States of Micronesia, Republic of Palau, and the Republic of the Marshall Islands).
Each year, approximately 1,500 Grants to States projects support the purposes and priorities outlined in the Library Services and Technology Act (LSTA; 20 U.S.C. § 9121). SLAAs may use the funds to support statewide initiatives and services, and they may also distribute the funds through competitive subawards to, or cooperative agreements with, public, academic, research, school, or special libraries or consortia (for-profit and federal libraries are not eligible).
While the projects listed below are not specifically in place to implement the Autism CARES Act of 2019, they are related to libraries’ efforts to serve people with autism and related developmental disabilities. Each link provides access to details about the project. Each award covers up to two years of activities; thus, these listings for 2019 and 2020 represent those for which final reports have been completed and submitted.
Access for All
(Sunderland Public Library, Massachusetts)
The Sunderland Public Library reimagined services to children on the autism spectrum and their families in ways that will invite them into the library, make them more comfortable spending time at the library, and make them feel like a valuable part of the community. These goals were accomplished by hiring consultants to assist in making services and facilities more accessible for people on the autism spectrum, developing programs that serve children on the autism spectrum, developing a sensory toy collection, redeveloping resources on autism, and redoubling efforts to reach out to children on the autism spectrum and their caregivers.
Youth Services
(State Library of North Carolina, North Carolina)
The Youth Services Programming offered learning opportunities for library staff that followed current research and trends to inform North Carolina youth programming and help libraries create and promote partnerships within their communities. For example, after one program, Taking Autism to the Library, participants remarked in evaluations that they gained a great deal of understanding on how to incorporate autism-friendly structures into their spaces, programs, and activities.
Sensory Backpacks: Young Learners of the Heart
(Nueces County Keach Family Library, Texas)
Nueces County Keach Family Library initiated sensory backpacks (Young Learners of the Heart) in Pop Pop’s Place at Robstown, Texas, to provide an all-in-one take-home kit for families that are designed to help children build life skills, social skills, and reading comprehension. The backpacks were designed to help children on the autism spectrum or sensitive to sensory overload by providing books, writing activities, tips for caregivers, and sensory items. The program included Sensory Storytime and materials to expand informational literacy and help the youth become lifelong learners. The program targeted area youth up to 19 years of age, lower income, at-risk teens, and those with intellectual disabilities with the goal of providing them access and instruction in using current book subjects on mindfulness, sensitivity, and anxiety.
Libraries on the Spectrum
(County of Imperial Free Library, California)
The Libraries on the Spectrum project sought to encourage families with individuals with autism to access their local public library for educational and recreational programs, specially curated resources, and to expand their personal networks in a comfortable and welcoming environment. The five participating local public library systems (Imperial County Free Library, Brawley Public Library, Camarena Memorial Library, El Centro Public Library, and Imperial Public Library) were on their way to achieving these goals when the COVID-19 pandemic abruptly halted and delayed activities.
Spotlight on Early Learning and Sensory Storytimes
(Kansas City Public Library, Missouri)
The Kansas City Public Library updated each branch's early literacy space to be more welcoming and inclusive for all children and held training for staff on working with children with sensory issues.
Public Library Association Conference 2020
(Saint Joseph Public Library, Missouri)
The Outreach Librarian at St. Joseph Public Library attended the 2020 Public Library Association Conference, February 25 – March 1, 2020, in Nashville, Tennessee. The participant's learning goals were to find new ways to reach out to their elderly, homeless, and underserved patrons. The attendee will use the knowledge gained to implement new or fine-tune existing programs to reach these special populations.
CAP Grants
(Arizona State Library, Archives and Public Records, Arizona)
The Arizona State Library awarded 19 Collections And Programming (CAP) mini-grants to 17 public and school libraries. These awards of $4,000 each were used to expand collections for a target audience and to increase access to those collections through programs. The primary purpose of CAP mini-grants is to provide resources for community members with defined needs such as at-risk children, the aging population, people having difficulty using the library, and others targeted in the LSTA priorities.
PaLA, College and Research Division Professional Development
(Pennsylvania Library Association, Pennsylvania)
This grant supported two primary, annual professional development opportunities for academic librarians, which focused on timely topics, featured national and regional speakers, and provided strategies that librarians can actively implement in their libraries to better serve their campus communities. Subjects covered included Listening to Community Users, Safe Space in Academic Libraries, White Fragility (book discussion), Centering Student Voices, Academic Libraries and the Autism Spectrum Disorder, Academic Freedom and Academic Libraries, Setting the Stage for Civic Minded Education, Health Information for Distance Learning, and Providing Services during COVID-19.
Beyond Access: Inclusive Programs at Mission Viejo Library
(Mission Viejo Public Library, California)
The Beyond Access project conducted a needs assessment of and with the disabled community in the Mission Viejo service area and provided pertinent training for library staff in order to develop inclusive programs and services now and in the future. The goal of this project was to identify the needs of the disabled community and equip library staff to make library and city services more inclusive and accessible in accordance with those identified needs, thereby improving the ability of the disabled community members to participate in the exceptional programs offered in Mission Viejo.
Libraries on the Spectrum
(County of Imperial Free Library, California)
The Libraries on the Spectrum Project encouraged families with individuals of all ages with autism to access their local public library to attend educational and recreational programs, borrow resources, and expand their personal networks in a library environment designed to be more comfortable and welcoming. All five public libraries in Imperial County circulated a collection of autism-specific resources and tools and provided targeted programming to benefit families with autism.
Sensory Inclusive Library Initiative
(Clay County Public Library System, Florida)
The Clay County Public Library System offers a welcoming and comfortable learning environment for individuals on the autism spectrum, their families, teachers, students, and therapeutic support specialists. The Accessibility Support Collection containing books, audio, DVDs, and other resources devoted to teaching social skills, behavioral therapy, conflict resolution, and community awareness was developed. Sensory backpacks were purchased and made available in each library location. The backpacks contained items that will be helpful to persons experiencing sensory overload.
Sensory Storytime
(Iredell County Library, North Carolina)
The Iredell County Public Library created sensory storytime kits for children on the autism spectrum and/or with sensory processing issues. By partnering with the Iredell County Partnership for Young Children, staff received training and tips on best practices for sensory storytime. The sensory kits are available for any patron to check out.
CE: Library Services and Programs Development
(Missouri State Library, Missouri)
The Missouri State Library held eleven live webinars that related to developing strong library programs and practices including Serving Patrons on the Autism Spectrum, Compassion Fatigue, Self-Care for Library Staff During the Pandemic, a four-part series on digital literacy for seniors, two workforce development programs, and Developmentally Appropriate Programming for Toddlers. Each webinar was archived for later viewing.
Youth Services Family Engagement
(Idaho Commission for Libraries, Idaho)
The Idaho Commission for Libraries (ICfL) has encouraged Idaho public and school libraries to reach out to underserved families in their communities through program activities, as well as through topic-specific grant work. Through the Welcoming Libraries Grant (WLG), the ICfL supports the assessment of equity, diversity, and inclusion (EDI) needs within their communities and libraries and funds small, related library improvements with $500 grants. Participating libraries were encouraged to work with at least one local partner to help them implement the grant activities. Partner examples include Idaho Educational Services for the Deaf and Blind, Coeur d’Alene Tribal Language Department, Panhandle Autism Society, Talk to Me Technologies, and the Green Apple Project. The Commission also provided an extensive EDI webpage of curated resources from other state and local libraries across the country that are doing significant EDI work. WLG activities offered this grant period included expansion of a sensory-friendly room at a library for therapy/program use as well as individual use.
Statewide Continuing Education
(Nevada State Library, Archives and Public Records, Nevada)
The Continuing Education project supports the professional development of Nevada’s public, academic, special, and school library staff, volunteers, and trustees. The Nevada State Library has undertaken to provide professional development and promote national best practices for 21st Century librarianship through a number of avenues, including offering scholarships to trainings and conferences; and procuring prepaid real-time and asynchronous online course seats. Online seats/courses topics included Weeding, Cataloging, Civil Legal Justice, Teen Services, Storytimes, LGBTQ Families, Social Media, Autism Spectrum Patrons, Diverse Collections, and Time Management.
In addition to projects funded through the Grants to States Programs, IMLS also funds projects relevant to individuals with autism and other disabilities through National Leadership Grants for Libraries, CARES Act Grants for Museums and Libraries, and the American Rescue Plan for Museums and Libraries.
In FY 2020, the University of Washington Information School conducted research aimed at improving libraries’ capacity to include children with autism and their families in early literacy programming. Funded by IMLS through a National Leadership Grant for Libraries and in partnership with the Seattle Children’s Autism Center, the Association for Library Services to Children, Seattle Public Library, and Pierce County Libraries, researchers at the University of Washington developed the Autism-Ready Libraries Toolkit, which includes free online training modules and resources for youth-serving librarians and library staff in public libraries who would like to better serve families with children on the autism spectrum.
The Intrepid Sea, Air & Space Museum received funding in FY 2020 through an IMLS CARES Act Grant for Museums and Libraries to develop easily accessible resources that was shared throughout the state of New York to support virtual education programming for approximately 12,000 New York residents over the span of two years. These virtual education programs and resources were geared toward high-need audiences of different ages and abilities, including individuals with autism or other developmental disabilities. One product of this grant is the publication Making History Accessible: Toolkit for Multisensory Interpretation, which offers a range of digital and physical/tactile solutions to help make interpretive content at historic sites and other educational facilities more accessible.
In FY 2022, IMLS provided funding through the American Rescue Plan for Museums and Libraries for Amazement Square, a children’s museum in Lynchburg, Virginia, to facilitate a comprehensive program addressing social-emotional and academic learning loss from the COVID-19 pandemic for children with autism and their families. The program will include a community advisory committee, in-class curriculum, exclusive quarterly museum experiences, professional development for museum staff, and publicly accessible digital resources. The program will increase the understanding of science, technology, engineering, arts, and math concepts among participating children; facilitate conversations and program development among the advisory committee; expand museum staff knowledge of inclusivity and autism programming; and heighten awareness of the museum’s accessibility resources.
The Indiana University Museum of Archaeology and Anthropology also received funding from IMLS in FY 2022 through the American Rescue Plan for Museums and Libraries to broaden its community involvement and service by removing barriers and providing resources and support for community members with invisible disabilities such as autism, sensory processing disorder, anxiety, agoraphobia, and depression. To achieve these goals, the museum will deliver programming for learners of all ages with varying needs and create a multifunctional wellness room, programming designed for neurodiverse visitors, and guides and sensory maps.
While IMLS does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, resources and services funded by IMLS are relevant to individuals on the autism spectrum and their families. These resources and services are intended to improve well-being, including for autistic individuals, across the lifespan, which is an over-arching theme of the recommendations in the IACC Strategic Plan. In addition, IMLS funds research and services activities relevant to Question 5 (Services) and Question 6 (Lifespan) of the IACC Strategic Plan. Though IMLS is not currently a member of the IACC or the FIWA, IMLS contributed to this report and the most recent IACC Portfolio Analysis Report.
National Aeronautics and Space Administration (NASA)
The National Aeronautics and Space Administration (NASA) is responsible for unique scientific and technological achievements in human spaceflight, aeronautics, space science, and space applications that have had widespread impacts on our nation and the world. While NASA does not receive funding from the Autism CARES Act of 2019, NASA programs support individuals with autism and other developmental disabilities in science education and employment.
Experienced NASA educators at Sonoma State University, together with autism education specialists from the Education Development Center and informal education experts from the New York Hall of Science, are leading NASA’s Neurodiversity Network (N3), a five-year program that will provide a pathway to NASA participation and STEM (science, technology, engineering, and mathematics) employment for neurodiverse learners, with a focus on those on the autism spectrum. The project targets all four of the top-level goals for NASA’s Science Activation (SciAct) program:
- Enabling STEM education for a segment of the population that is significantly underserved by co-redeveloping existing NASA resources with autistic learners;
- Improving scientific literacy for this underserved population by providing authentic NASA experiences for autistic STEM learners;
- Partnering with autism-focused organizations to leverage efforts to create a sustainable pathway that provides autistic learners with the social and technical skills needed for successful STEM careers; and
- Working with autism experts to provide professional learning for subject matter experts and the NASA community around neurodivergence and best practices for working with autistic learners.
To target autistic learners and those with other learning differences, NASA educators and experts on ASD and informal learning will team with autistic learners to co-develop a cross-division SciAct program that will:
- Identify existing NASA resources that can be modified for accessibility;
- Modify and test the resources with autistic and other neurodiverse learners to ensure that they meet documented needs;
- Disseminate the resources through existing NASA SciAct groups, national youth networks, and autism-serving organizations;
- Conduct professional development for informal educators and SciAct members that work with youth groups to ensure that autistic learners are included in an equitable manner in activities;
- Conduct professional development for NASA Subject Matter Experts who will serve as mentors to autistic teens selected for internships; and
- Engage selected autistic teens in NASA-related internships.
NASA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan. However, NASA activities provide educational, internship, and employment opportunities for individuals on the autism spectrum and are relevant to Question 6 (Lifespan) of the IACC Strategic Plan. Though NASA is not currently a member of the IACC or the FIWA, NASA participates in efforts to coordinate autism activities across the federal government and contributed to this report.
National Endowment for the Arts (NEA)
Established by Congress in 1965, the National Endowment for the Arts (NEA) is an independent federal agency and the largest funder of the arts and arts education in communities nationwide and a catalyst of public and private support for the arts. By advancing equitable opportunities for arts participation and practice, the NEA fosters and sustains an environment in which the arts benefit everyone in the United States. While the NEA does not receive funding from the Autism CARES Act of 2019, the NEA funds several initiatives relevant to individuals on the autism spectrum and their families.
One of the core functions of the NEA is funding research into the value and impact of the arts, including on the use of art to advance health and well-being for autistic individuals. The NEA’s Research Labs initiative funds a transdisciplinary research team that seeks to address high unemployment among neurodiverse populations through the Autism Brilliance Lab for Entrepreneurship. This program examines how creativity in art and design serves as a vehicle for preparing populations on the autism spectrum for the workforce and preparing neurotypical work environments for people with autism. Another NEA Research Lab at Vanderbilt University conducted a randomized-waitlist control trial of a community-based music program (SeRenade) designed to foster active engagement of parents and children with autism through shared musical experiences and is now studying how different types and frequency of music training impacts parent-child outcomes.
In addition, the NEA commissioned a field scan specifically looking at disability as it relates to public space (including architecture, landscape architecture, urban design, and other public space design) and disability and the human body and mind (including fashion design, industrial design, and graphic design and computer science). Through the scan, the NEA sought to assess the current trends and needs of the disability design field, identify innovative programs and initiatives, and engage scholars and designers who are advancing the work. One prominent finding across design disciplines found that a number of disability communities are being left out of design discourse; among them are disabled BIPOC and those who identify as neurodiverse. The field scan summary report includes details of the findings and recommendations to address the needs of the disability communities.
Beyond research, NEA grantmaking supports various projects expanding access to and through the arts. Through the American Rescue Plan grant program, the NEA provided staff funding for the Spectrum Theatre Ensemble, a company of neurodiverse theatre artists based in Rhode Island that works to provide equitable opportunities for both neurodivergent and neurotypical people to engage with the theatre. Outside of relief funding programs, from FY 2019 to 2023, the NEA has funded 50 projects specifically related to individuals on the autism spectrum, totaling approximately $1.68 million in funding, as well as 67 projects more broadly relating to individuals with intellectual and developmental disabilities, totaling approximately $1.19 million in funding. Two examples are highlighted below.
- Through its principal funding program, Grants for Arts Projects, the NEA provided funding for New York City Board of Education - District 75 to support a Teaching Artist Training Institution. This project provided teachers, occupational, speech, and physical therapists with professional development training in music, theater, and visual arts instruction for students on the autism spectrum.
- The NEA has also supported organizations such as The Arc of Palm Beach County in Riviera Beach, Florida, to provide virtual and in-person art lessons for adults with intellectual and developmental disabilities. This project was funded through Challenge America, an NEA funding program supporting projects that extend the reach of the arts to communities that are underserved, including specifically those whose opportunities to experience the arts are limited relative to disability.
The NEA is committed to ensuring that everyone has access to the arts, including people with autism or other disabilities, and works to assist individuals and organizations in making their programs and facilities accessible and inclusive for people with disabilities and assist individuals with disabilities in connecting them with resources for access to the arts. The NEA’s Office of Accessibility is the advocacy-technical assistance arm of the NEA to make the arts accessible for people with disabilities, older adults, veterans, and people living in institutions. The office works in a variety of ways to accomplish its goals, including:
- Providing technical assistance to individuals and organizations to help open existing programs and make the arts accessible and inclusive for people with disabilities, older adults, and people living in institutional settings and to help organizations comply with the NEA’s Section 504 Regulations under the Rehabilitation Act and the ADA;
- Initiating cooperative projects with other federal agencies and nonprofit organizations to better educate professionals serving people with disabilities and older adults concerning access issues and the value and benefits of arts programming;
- Encouraging support for addressing the needs of people with disabilities and older adults through the NEA’s staff and through state and national organizations such as the 56 State and Jurisdictional Arts Agencies and six Regional Arts Organizations;
- Assisting applicants and grantees with the development of projects that involve the disability community, older adults, and people living in institutional settings; and
- Organizing and convening panels, seminars, and workshops for NEA staff, grantees, and other federal agencies.
The NEA’s Office of Civil Rights and Equal Employment Opportunity is responsible for the development, implementation, and coordination of all aspects of civil rights programs. For programs and activities receiving federal financial assistance from the NEA, this includes the administration of nondiscrimination statutes that prohibit discrimination on the basis of race, color, national origin, sex, age, or disability. This also includes prohibiting discrimination on the basis of disability in programs conducted by the NEA.
While the NEA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, services and resources provided by the NEA are available to individuals on the autism spectrum and their families. These services and resources are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. In addition, the NEA funds research and services activities relevant to Question 4 (Interventions), Question 5 (Services and Supports), and Question 6 (Lifespan) of the IACC Strategic Plan. Though NEA is not currently a member of the IACC or the FIWA, NEA participates in efforts to coordinate autism activities across the federal government and contributed to this report and the most recent IACC Portfolio Analysis Report.
National Science Foundation (NSF)
The mission of the National Science Foundation (NSF) is to promote the progress of science; to advance the national health, prosperity, and welfare; and to secure the national defense. NSF is the only federal agency whose mission includes support for all fields of fundamental science and engineering, except for medical sciences. While NSF does not have an ASD research program, the agency has awarded numerous research grants through the years that include basic science research with implications for the health and well-being of individuals with ASD and other developmental disabilities. These research awards, including current active awards, fall under a portfolio that emphasizes neuroscience, cognitive sciences, education and learning research, and workforce development. For example, NSF is currently funding two projects at Vanderbilt University to ensure that neurodiverse students can access and succeed in engineering majors and careers (2217621) and to train graduate students in a new interdisciplinary field which links human-technology frontiers research and education across STEM disciplines through a cohesive focus on autism (1922697). NSF is also funding a project to develop AI technologies to address cyberbullying and cybersecurity for adolescents with ASD (2114808; University of Central Florida), and the National AI Institute for Exceptional Education at the University of Buffalo, jointly funded by NSF and ED, is developing AI solutions to enable universal early screening and provide individualized interventions for children working with speech language pathologists (2229873).
NSF continues to encourage research related to individuals with disabilities, including autism, through direct outreach to the field. This includes two recent Dear Colleague Letters focused on disability: Research to Improve STEM Teaching, Learning, and Workforce Development for Persons with Disabilities (NSF 21-114) and Persons with Disabilities – STEM Engagement and Access (NSF 21-110). The NSF’s award search website offers the public the opportunity to learn about specific NSF awards.
NSF does not participate as a member agency on the IACC or the FIWA, but it has continued efforts to regularly monitor the funding of basic science and science education research about, and including, persons with ASD. NSF conducts searches of the IACC ARD to avoid funding duplication. NSF participates in the Interagency Committee on Disability Research as a statutory member, to monitor and contribute to interagency actions relevant to basic science and science education research about, and including, persons with disabilities. NSF also monitors the implementation and progress made on implementation related to the IACC Strategic Plan by virtually observing the quarterly IACC meetings, reviewing the relevant IACC reports, and examining the annual and final reports of NSF-funded projects about, and including, persons with ASD. While NSF does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, NSF funds research that address Question 1 (Screening and Diagnosis), Question 2 (Biology), Question 4 (Interventions), Question 5 (Services and Supports), Question 6 (Lifespan), and Question 7 (Infrastructure and Prevalence) of the IACC Strategic Plan.
Table 14: NSF basic science and science education funding related to, or including, persons with ASD.
| NSF Basic Science and Science Education Funding Related to ASD: FY 2019 – FY 2022 | ||
|---|---|---|
| Fiscal Year | Number of Awards | Total Obligations |
Fiscal Year2019 |
Number of Awards45 |
Total Obligations$19,801,919 |
Fiscal Year2020 |
Number of Awards50 |
Total Obligations$9,549,918 |
Fiscal Year2021 |
Number of Awards63 |
Total Obligations$14,999,447 |
Fiscal Year2022* |
Number of Awards19 |
Total Obligations$9,005,062 |
FY 2023 data was not available at the time this report was written.
* FY 2022 funding data is estimated.
Social Security Administration (SSA)
The mission of the Social Security Administration (SSA) is to ensure equity and accessibility in delivering Social Security services by improving the customer experience and addressing systemic barriers to participation in SSA programs. SSA administers two disability programs authorized under the Social Security Act – the Social Security Disability Insurance (SSDI) and the Supplemental Security Income (SSI) programs.
The SSDI program pays benefits to the disabled individual and certain family members if the beneficiary is "insured" (i.e., they have worked long enough – and recently enough – and paid Social Security taxes on their earnings). Those receiving SSDI benefits are also eligible for Medicare, generally after a 24-month qualifying period. The first 24 months of disability benefit entitlement is the waiting period for Medicare coverage. The SSI program provides financial assistance to meet basic needs for food, clothing, and shelter to adults and children with disabilities who have limited income and resources. SSI is funded by general tax revenues. In most states, SSI recipients qualify for Medicaid automatically without the need to fill out a Medicaid application or qualify after applying.
SSA evaluates claims relating to ASD for both adults (aged 18-64 years) and children (aged <18 years) under the SSDI and SSI programs, although neither of these programs are specifically in place to implement the Autism CARES Act of 2019. Generally, disability is not relevant when determining eligibility for the population over 65 for the SSI program or for Social Security retirement benefits; however, diagnosis is used for eligibility determinations for Disabled Adult Children (i.e., children of a Social Security beneficiary who are unmarried, age 18 or older, have a qualified disability that started before age 22, and meet the definition of disability for adults) regardless of age. While the SSDI and SSI programs are different, the medical requirements are the same. Individuals may claim benefits under both programs concurrently.
SSA follows a five-step sequential process for evaluating adult disability claims:
- Consider whether the adult is engaging in substantial gainful activity.
- Consider whether the person has a severe medically determinable impairment. At this step, SSA considers the diagnosis of ASD in conjunction with the medical and other evidence to establish the medically determinable impairment and its severity.
- Consider whether the severe medically determinable impairment(s) meets or medically equals one of the listings. At this step, ASD is considered under mental disorders listing 12.10 in 20 CFR Part 404, Subpart P, Appendix 1. If the adult does not have an impairment that meets or medically equals a listing, SSA determines the residual functional capacity (RFC) resulting from the ASD and any coexisting medically determinable impairments.
- Determine whether the person’s RFC would permit the person to perform any past relevant work the individual may have.
- Determine whether the person’s RFC would permit the individual to perform any other work that exists in the national economy.
SSA follows a three-step sequential process for evaluating child disability claims:
- Consider whether the child is engaging in substantial gainful activity.
- Determine whether the child has a severe medically determinable impairment that meets or medically equals a listing. At this step, ASD is considered under mental disorders listing 112.10 in 20 CFR Part 404, Subpart P, Appendix 1.
- Determine whether the child’s ASD and coexisting medically determinable impairment(s) functionally equal the listings, using the whole-child approach.
As of December 2021, approximately 418,000 individuals with a primary impairment of ASD – approximately 215,000 children (under 18 years of age) and 203,000 adults (18-64 years of age) – received SSI payments. Children received an average monthly payment of $678, and adults received an average monthly payment of $652. In addition, approximately 110,000 SSDI beneficiaries had a primary impairment of ASD, of whom 27% were workers and 73% were adult children. Workers received an average monthly payment of $804, and adult children received an average monthly payment of $957. Out of approximately 275,000 total adult recipients with a primary impairment of ASD, 62% received SSI only, 26% received SSDI only, and 12% received both SSI and SSDI.
In calendar year 2021, SSA processed 22,742 first-time adult and 29,738 first-time child claims for ASD. Of those claims, 71% of adult claims and 73% of child claims met requirements following initial determination/reconsideration and were allowed benefits, compared to 39% and 48%, respectively, for all impairments.
SSA also runs the Ticket to Work program. This is a free and voluntary program that connects eligible individuals with free employment services. It is available to everyone age 18 through 64 who receives SSDI and/or SSI benefits because of the individual’s disability. Through an alternative program, SSA reimburses state VR agencies for services provided to beneficiaries who successfully return to work. Of the 342,369 SSDI and/or SSI beneficiaries with either a primary or secondary diagnosis of ASD who were either receiving payments or whose payments were suspended due to their wage income in 2020, 89,701 (26.2%) had participated in the Ticket to Work program and used either Employment Networks or state VR agency services at some point while receiving benefits.
SSA is running a national targeted campaign to reach people who may be eligible for the SSI program, including people facing barriers, especially those with low income, limited English proficiency, facing homelessness, or with mental illness. In addition, SSA joined with external partners to launch a new national outreach campaign to connect eligible individuals to SSI and SSDI benefits. The SSI and SSDI programs provide critical financial assistance, including life-saving access to health care and the Supplemental Nutrition Assistance Program in many cases. Key components of SSA’s ongoing outreach campaign are:
- Working with community-based groups that can assist with taking applications for SSI and SSDI;
- Launching a national advertising campaign on TV, radio, and social media, with emphasis on children with disabilities; and
- Adding online tools and informational pages, including online resources for people helping others access SSA services, outreach materials for people facing barriers for use by partner groups, and information for faith-based and community groups, including a new toolkit and fact sheets about SSI and SSDI.
SSA conducts numerous research and demonstration projects to study ways to improve services to current and future Social Security beneficiaries. SSA supports several demonstrations and projects intended to address the broad needs of beneficiaries with disabilities. These projects can lead to ways to better serve individuals with disabilities, including potentially changing program rules to allow for better coordination among other federal and state programs. The Administration also receives funding for projects through specific congressional mandates. These projects support specific program changes or outreach activities targeted to populations in particular need. SSA held a virtual state of the science meeting in 2021 to discuss the lessons learned from past demonstrations. To find out more about the event and access a digital copy of the associated volume, see the Lessons Learned from SSA Demonstrations page.
One example of demonstration that did not focus on ASD but is still informative was the Promoting Readiness of Minors in SSI (PROMISE) project, a collaboration between SSA and the Departments of Education, Labor, and Health and Human Services. The effort tested services for children ages 14-16 receiving SSI and their families, targeted at supporting improved employment, education, and other outcomes. One report from PROMISE specifically looked at participants with ASD found that 13% of youth participants in PROMISE had a primary diagnosis of ASD in SSA’s systems. The report found that services available to participants with ASD existed but were not always received and that the program had positive impacts on service receipt and earnings.
SSA’s Analyzing Relationships between Disability, Rehabilitation, and Work (ARDRAW) Small Grant Program is a one-year $10,000 stipend program awarded to graduate-level students to conduct supervised independent research designed to foster new analysis of work, rehabilitation, and disability issues, which may develop innovative and fresh perspectives on disability. ARDRAW focuses on research relevant to SSA’s work incentives and employment supports – specifically rehabilitation, work, and the disability program. Examples of ARDRAW grants that have focused specifically on improving employment outcomes for individuals on the autism spectrum include:
- Workplace and Interview Disclosure Strategies for Adults with Autism Spectrum Disorder Eligible for Social Security Benefits: An Analysis of Employer, Employee and Applicant Experiences (George Washington University)
- COVID-19 and Mobility Impacts on Employment of Adult Social Security Beneficiaries with Autism Spectrum Disorder (Temple University)
The Retirement and Disability Research Consortium (RDRC) is an interdisciplinary extramural research program funded through five-year cooperative agreements. Through RDRC, SSA funds research on a wide array of topics related to Social Security's Old-Age, Survivors, and Disability Insurance and SSI programs and related federal policies, including topics related to autism.
The Interventional Cooperative Agreement Program (ICAP) allows SSA to enter into cooperative agreements to collaborate with states, private foundations, and other non-federal groups and organizations who have the interest and ability to identify, operate, and partially fund interventional research related to the Disability Insurance and SSI programs. SSA's demonstration authority for ICAP is derived from Section 1110 [42 U.S.C. § 1310] of the Social Security Act. ICAP is an ongoing program that will request new applications for award on a regular basis. In 2022, ICAP made awards to Mathematica and Westat that will likely benefit those on the autism spectrum. Mathematica is conducting a randomized controlled trial to assess the impact of an employment intervention for youth with disabilities who are transitioning into the adult workforce. Westat is conducting a randomized controlled trial to assess the impact of combining supportive housing with Individual Placement and Support supported employment services for recently homeless people experiencing a range of disabilities and mental health conditions.
While SSA does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan, SSA-funded research addresses Question 5 (Services and Supports) and Question 6 (Lifespan) of the IACC Strategic Plan. SSA additionally funds services and activities, described above, that broadly impact individuals with disabilities, including those with ASD and their families. These activities are intended to improve health and well-being, including for autistic individuals, across the lifespan, which is an overarching theme of the recommendations in the IACC Strategic Plan. SSA is a member of the IACC and the FIWA and participates in efforts to coordinate autism activities across the federal government.
U.S. Agency for International Development (USAID)
The U.S. Agency for International Development (USAID) leads the U.S. government’s international development and disaster assistance efforts through partnerships and investments that save lives, reduce poverty, strengthen democratic governance, and help people emerge from humanitarian crises and progress beyond assistance. USAID’s investments in global health continue to prioritize interventions which directly address the leading causes of maternal and child morbidity and mortality, including focus areas in maternal and newborn health; child health; immunization; nutrition; water, sanitation, and hygiene; malaria; family planning and reproductive health; health systems strengthening; and monitoring, evaluation, research, and learning to identify barriers and solutions to prevent child and maternal deaths. USAID generally does not undertake programs that target children with specific non-communicable diseases or neurological disorders. USAID global health funding for maternal and child health focuses on programs that reduce mortality, including essential newborn care, prevention and treatment of diarrheal disease, and efforts to impact child survival.
USAID is committed to the inclusion of people who have physical and cognitive disabilities and is investing in programs supporting this population. One such program is the Disability Program Fund. Since 2005, USAID’s Disability Program Fund has supported more than 150 programs and activities in 65 countries, working with various organizations and implementing partners. In many instances, these organizations are Disabled People's Organizations, civil society organizations run by and for persons with disabilities. Programming areas include democracy, human rights, and governance; economic growth and trade; and education; among others. Through its Disability Program Fund and broader inclusive development efforts, USAID is working with the disability community around the world to ensure that persons with disabilities are empowered to fully exercise their human rights on an equal basis with others. Some program highlights are listed below.
- Art for Inclusion of Persons with Disabilities increases inclusion and improves the quality of life of children and young persons with disabilities in Belarus through launching awareness-raising campaigns, strengthening a network of local disabled people’s organizations, and developing social enterprises and community-based services. The project promotes the rights of persons with disabilities and their inclusion in society through artistic and other events. Activities also aim to engage new grassroots Disabled People’s Organizations in networking and exchanging experiences and lessons learned.
- All Children Reading Cambodia improves early grade learning skills of children, including children with disabilities in grades one to three. Outcomes include meaningful participation of children with disabilities in the learning process with improved performance, writing, and mathematics.
- Expanding Employment and Income-Generation Opportunities for Persons with Disabilities provides persons with disabilities with new climate-adaptive technologies and financing that will help them generate income and participate in the economy. The program works to integrate persons with disabilities into programs and initiatives to improve food security in the region.
USAID initiatives in Vietnam are currently focused on providing services for persons with significant disabilities, regardless of cause, in areas heavily sprayed with Agent Orange, part of the U.S. government’s efforts to address the legacies of the U.S.-Vietnam War. Over the last 30 years, projects have contributed to the improvement of the quality of life of persons with disabilities in Vietnam, with impacts including:
- Direct support to over 46,000 persons with disabilities;
- Improved rehabilitation and social services for persons with disabilities;
- Improved disability policy and advocacy; and
- Improved partners’ capacity in management, implementation, and activity support to persons with disabilities.
Some USAID support has directly assisted those with intellectual and developmental disabilities, including children with autism. Through programs such as I-THRIVE, USAID has supported specialized caregiver training for parents and health professionals; advocacy efforts by the Vietnam Association of Parents with Kids with Autism; and health system improvements on early identification, diagnosis, and intervention for children with autism. Meanwhile, Vietnamese children and adults with autism have also benefited from USAID-championed disabilities policy reforms that have improved health care access and educational opportunities and reduced social stigma towards all persons with disabilities.
USAID does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan. However, services and resources provided by USAID are intended to improve health and well-being, including for autistic individuals, across the lifespan. USAID activities are also relevant to Question 1 (Screening and Diagnosis), Question 4 (Interventions), Question 5 (Services and Supports), and Question 6 (Lifespan) of the IACC Strategic Plan. Though USAID is not currently a member of the IACC or the FIWA, USAID participates in efforts to coordinate autism activities across the federal government and contributed to this report.
U.S. Geological Survey (USGS)
The U.S. Geological Survey (USGS) is the science arm of the Department of the Interior and provides science for a changing world, which reflects and responds to society’s continuously evolving needs. The USGS brings an array of earth, water, biological, and mapping data and expertise to bear in support of decision-making on environmental, resource, and public safety issues. While the USGS does not receive funding from the Autism CARES Act of 2019, USGS programs support individuals with autism and other developmental disabilities in science education and employment transition.
The USGS’s Office of Science Quality and Integrity promotes diversity, equity, and inclusion through a variety of programs that target the spectrum of learners from early childhood through post-doctoral fellowships, including youth with autism and other developmental disabilities. The College Partnerships in Neurodiversity USGS program supports student internships at USGS centers that are close to partner colleges. Paid internships for students offer professional development in science and workplace experience to help neurodiverse students transition into the workforce.
The USGS collaborates with school districts and other educational institutions that have work transition programs for students with cognitive and other disabilities through the Secondary Transition to Employment Program – USGS Partnership (STEP-UP). Through the partnership, students have training experiences with the USGS to gain valuable job skills to support their goals of seeking employment and living independently. The students engage in projects that involve sorting, counting, comparing, cataloging, and identifying and tagging information in various data sets from the different mission areas in the USGS. Many students assist in the preservation of at-risk data by scanning paper and other analog records and adding important metadata. The students’ contributions benefit the USGS, the larger scientific community, and the public by making information more accessible.
The USGS does not receive funding specifically to implement the Autism CARES Act of 2019 or the IACC Strategic Plan. However, USGS activities provide educational, internship, and employment opportunities for individuals on the autism spectrum and are relevant to Question 6 (Lifespan) of the IACC Strategic Plan. Though the USGS is not currently a member of the IACC or the FIWA, the USGS participates in efforts to coordinate autism activities across the federal government and contributed to this report.
Prevalence of Autism Spectrum Disorder
This portion of the report covers Section 399DD(a)(2)(C) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which requires: (C) "Information on the incidence and prevalence of autism spectrum disorder, including available information on the prevalence of autism spectrum disorder among children and adults, and identification of any changes over time with respect to the incidence and prevalence of autism spectrum disorder." Information on the prevalence of ASD is provided by the HHS’s CDC and HRSA, as well as ED and EPA.
Department of Health and Human Services (HHS)
Centers for Disease Control and Prevention (CDC)
CDC's ADDM Network provides important information on the numbers of children identified with ASD and helps describe the characteristics of the population. Surveillance tracks trends over time and is an essential building block for population-based research, providing clues about potential risk factors that warrant further study. Surveillance also provides critically important data for communities to use when planning for services.
The ADDM Network has estimated prevalence of ASD among 8-year-old children every two years since 2000 in different communities located across the United States. States and territories that have participated in at least one surveillance year as of April 2023 are Alabama, Arizona, Arkansas, Colorado, Florida, Georgia, Indiana, Maryland, Minnesota, Missouri, New Jersey, North Carolina, Pennsylvania, Puerto Rico, South Carolina, Tennessee, Texas, Utah, West Virginia, and Wisconsin. ADDM Network data have shown significant variation in ASD prevalence among 8-year-old children by geographic area, sex, race/ethnicity, and level of intellectual ability.
In 2020, ASD prevalence estimates varied across the 11 ADDM communities, ranging from 1 in 43 children in Maryland to 1 in 22 children in California. There is no evidence to suggest that living in certain communities puts children at greater risk for ASD; these variations more likely reflect community practices and the available resources for identifying children with ASD. Data from the ADDM Network show an increase in the identified prevalence of ASD between 2000 (6.7 per 1,000 children) and 2020 (27.6 per 1,000 children). These results are based on the average prevalence from all participating sites during a specific year; however, the composition of sites and the specific geographical areas within each site have varied over time.
The prevalence of ASD has been consistently higher among boys than girls in the ADDM Network. In the most recent ADDM report released in 2023, the ratio was four boys with ASD identified for every one girl with ASD identified. For the first time since ADDM reporting began, the percentage of girls identified with ASD was over 1%.
Prior to surveillance year 2016, the percentage of children identified with ASD by 8 years of age in the ADDM Network was higher among White children than among Asian or Pacific Islander, Black, and Hispanic children. In recent years, differences in identification of autism by race and ethnicity began to narrow until there was no overall difference observed between groups in surveillance year 2018. However, in surveillance year 2020, the percentage of 8-year-old Asian or Pacific Islander (3.3%), Hispanic (3.2%) and Black (2.9%) children identified with autism was higher than among 8-year-old White children (2.4%) for the first time. While this new pattern could suggest improvements in equitable identification of autism, it’s too early to know the cause of this shift.
In surveillance year 2020, 37.9% of children with ASD had co-occurring intellectual disability in the ADDM Network. This represents a decrease from the estimated 40-62% of children with ASD who were diagnosed with a co-occurring intellectual disability in 2000.55 The decrease is likely due to the increase in diagnosis of autism in children with average to above average cognitive function. A higher percentage of 8-year-old Black children (50.8%) with autism had intellectual disability compared to 8-year-old Asian or Pacific Islander (41.5%), Hispanic (34.9%) or White (31.8%) children with ASD. These differences could relate in part to access to services that diagnose and support children with ASD.
In 2020, CDC used statistical modeling to estimate national and state prevalence of adults 18-84 years living with ASD.2 Based on data in 2017, the model estimates that approximately 2.21% or 5.4 million U.S. adults aged 18 and older have ASD, with state prevalence ranging from 1.97% in Louisiana to 2.42% in Massachusetts.
Table 15: ASD prevalence data from CDC’s ADDM Network, 2000-2020, combining data from all sites.
| CDC ADDM Network ASD Prevalence Data: 2000 – 2020 | ||||
|---|---|---|---|---|
| Surveillance Year | Birth Year | Number of ADDM Sites Reporting | Prevalence per 1,000 Children (Range) | This is approximately one in X children |
Surveillance Year2000 |
Birth Year1992 |
Number Of ADDM Sites Reporting6 |
Prevalence Per 1,000 Children (Range)6.7 (4.5-9.9) |
This is Approximately One in X Children1 in 150 |
Surveillance Year2002 |
Birth Year1994 |
Number Of ADDM Sites Reporting14 |
Prevalence Per 1,000 Children (Range)6.6 (3.3-10.6) |
This is Approximately One in X Children1 in 150 |
Surveillance Year2004 |
Birth Year1996 |
Number Of ADDM Sites Reporting8 |
Prevalence Per 1,000 Children (Range)8.0 (4.6-9.8) |
This is Approximately One in X Children1 in 125 |
Surveillance Year2006 |
Birth Year1998 |
Number Of ADDM Sites Reporting11 |
Prevalence Per 1,000 Children (Range)9.0 (4.2-12.1) |
This is Approximately One in X Children1 in 110 |
Surveillance Year2008 |
Birth Year2000 |
Number Of ADDM Sites Reporting14 |
Prevalence Per 1,000 Children (Range)11.3 (4.8-21.2) |
This is Approximately One in X Children1 in 88 |
Surveillance Year2010 |
Birth Year2002 |
Number Of ADDM Sites Reporting11 |
Prevalence Per 1,000 Children (Range)14.7 (5.7-21.9) |
This is Approximately One in X Children1 in 68 |
Surveillance Year2012 |
Birth Year2004 |
Number Of ADDM Sites Reporting11 |
Prevalence Per 1,000 Children (Range)14.6 (8.2-24.6) |
This is Approximately One in X Children1 in 68 |
Surveillance Year2014 |
Birth Year2006 |
Number Of ADDM Sites Reporting11 |
Prevalence Per 1,000 Children (Range)16.8 (13.1-29.3) |
This is Approximately One in X Children1 in 59 |
Surveillance Year2016 |
Birth Year2008 |
Number Of ADDM Sites Reporting11 |
Prevalence Per 1,000 Children (Range)18.5 (13.1-31.4) |
This is Approximately One in X Children1 in 54 |
Surveillance Year2018 |
Birth Year2010 |
Number Of ADDM Sites Reporting11 |
Prevalence Per 1,000 Children (Range)23.0 (16.5-38.9) |
This is Approximately One in X Children1 in 44 |
Surveillance Year2020 |
Birth Year2012 |
Number Of ADDM Sites Reporting11 |
Prevalence Per 1,000 Children (Range)27.6 (23.1-44.9) |
This is Approximately One in X Children1 in 36 |
Health Resources and Services Administration (HRSA)
Information about health care access among children and youth with autism and developmental disabilities is available from the HRSA-funded and directed NSCH. The NSCH is an annual, nationally representative survey that provides a unique source of national and state-level data on child health and health care, including health care access for children and youth with autism and developmental disabilities. The NSCH collects parent-reported information on whether the child ever received an autism diagnosis by a care provider, current autism status, health care use, access and challenges, and methods of treatment.
Data from the 2020-2021 NSCH indicates that approximately 1 in 40 children in the United States are currently diagnosed with autism, with an overall prevalence of 2.9% among children ages 3-17 years. This rate remained stable between 2016 and 2021.56 Research using prior iterations of the NSCH found the prevalence of autism to be higher among boys compared to girls. Autism prevalence was also found to be higher for children with single mothers compared to children in two-parent, married households. In addition, children from households with income less than 100% of the federal poverty level were also more likely to be diagnosed with ASD compared to children from households at more than 400% of the federal poverty level. ASD prevalence was also found to be higher among children born preterm rather than at term.57
Department of Education (ED)
OSEP within ED collects data from states on the number of students with ASD that receive services under IDEA, Part B (Tables 16 and 17). These and other data are reported in the IDEA Section 618 data files and statistics tables, as well as the 44th Annual Report to Congress.
From 2012 through 2021, children ages 6-11 made up the largest age group served under the IDEA, Part B, and reported under the category of autism (Table 16 and Figure 1). Between 2012 and 2021, the percentages of the populations ages 12-17 and 18-21 served under the IDEA, Part B, that were reported under the category of autism both increased and were 86% and 81% larger in 2021 than in 2012, respectively (Figure 1).
Table 16: Number of children ages 5 (school age) – 21 with autism served under the IDEA, Part B, by year for fall 2012 through fall 2021.
| Number of Children Served under the IDEA, Part B: Fall 2012 – Fall 2021 | ||||||
|---|---|---|---|---|---|---|
| Year | Ages 5 (School Age) – 11 | Ages 6-11 | Ages 12-17 | Ages 18-21 | Ages 5 (School Age) – 21 | Ages 6-21 |
Year2012 |
Ages 5 (School Age) – 11N/A |
Ages 6-11231,165 |
Ages 12-17179,020 |
Ages 18-2133,809 |
Ages 5 (School Age) – 21N/A |
Ages 6-21443,994 |
Year2013 |
Ages 5 (School Age) – 11N/A |
Ages 6-11244,272 |
Ages 12-17198,653 |
Ages 18-2136,058 |
Ages 5 (School Age) – 21N/A |
Ages 6-21478,983 |
Year2014 |
Ages 5 (School Age) – 11N/A |
Ages 6-11257,714 |
Ages 12-17217,960 |
Ages 18-2138,014 |
Ages 5 (School Age) – 21N/A |
Ages 6-21513,688 |
Year2015 |
Ages 5 (School Age) – 11N/A |
Ages 6-11271,175 |
Ages 12-17238,607 |
Ages 18-2140,623 |
Ages 5 (School Age) – 21N/A |
Ages 6-21550,405 |
Year2016 |
Ages 5 (School Age) – 11N/A |
Ages 6-11282,842 |
Ages 12-17252,477 |
Ages 18-2143,446 |
Ages 5 (School Age) – 21N/A |
Ages 6-21578,765 |
Year2017 |
Ages 5 (School Age) – 11N/A |
Ages 6-11301,740 |
Ages 12-17267,721 |
Ages 18-2146,773 |
Ages 5 (School Age) – 21N/A |
Ages 6-21616,234 |
Year2018 |
Ages 5 (School Age) – 11N/A |
Ages 6-11326,905 |
Ages 12-17285,801 |
Ages 18-2151,138 |
Ages 5 (School Age) – 21N/A |
Ages 6-21663,844 |
Year2019* |
Ages 5 (School Age) – 11362,062 |
Ages 6-11N/A |
Ages 12-17301,595 |
Ages 18-2154,059 |
Ages 5 (School Age) – 21717,716 |
Ages 6-21N/A |
Year2020 |
Ages 5 (School Age) – 11392,873 |
Ages 6-11N/A |
Ages 12-17317,723 |
Ages 18-2157,583 |
Ages 5 (School Age) – 21768,179 |
Ages 6-21N/A |
Year2021 |
Ages 5 (School Age) – 11434,604 |
Ages 6-11N/A |
Ages 12-17332,549 |
Ages 18-2161,257 |
Ages 5 (School Age) – 21828,410 |
Ages 6-21N/A |
Data for 2022 and 2023 was not available at the time this report was written.
* Beginning in 2019, child counts reporting categories changed from 6-11 to 5-11 and from 6-21 to 5-21.
Table 17: Percent of the population ages 6 through 21 (2006-2018) or 5 through 21 (2019-2021) with autism served under the IDEA, Part B, by year for fall 2006 through fall 2021.
| Percent of the Population with Autism Served under the IDEA, Part B: 2006 – 2021 | |
|---|---|
| Year | Percent of Total Population |
Year2006 |
Percent of Total Population0.3 |
Year2007 |
Percent of Total Population0.4 |
Year2008 |
Percent of Total Population0.4 |
Year2009 |
Percent of Total Population0.5 |
Year2010 |
Percent of Total Population0.5 |
Year2011 |
Percent of Total Population0.6 |
Year2012 |
Percent of Total Population0.7 |
Year2013 |
Percent of Total Population0.7 |
Year2014 |
Percent of Total Population0.8 |
Year2015 |
Percent of Total Population0.8 |
Year2016 |
Percent of Total Population0.9 |
Year2017 |
Percent of Total Population0.9 |
Year2018 |
Percent of Total Population1.0 |
Year2019* |
Percent of Total Population1.1 |
Year2020 |
Percent of Total Population1.1 |
Year2021 |
Percent of Total Population1.14 |
Data for 2022 and 2023 was not available at the time this report was written.
Percentage was calculated by dividing the number of students ages 6-21 (or 5-21) served under the IDEA, Part B, in the disability category in the year by the estimated U.S. resident population ages 6-21 (or 5-21) for that year, then multiplying the result by 100.
* Beginning in 2019, child counts reporting categories changed from 6-21 to 5-21.
Figure 1. Percentage of the population ages 6 through 21 (2011-2019) or 5 (school age) through 21 (2020) served under the IDEA, Part B, that was reported under the category of autism by year and age group for fall 2011 through fall 2020.
Data for 2021-2023 was not available at the time this report was written.
Percentage was calculated by dividing the number of students in the age group served under the IDEA, Part B, who were reported under the category of autism in the year by the estimated U.S. resident population in the age group for that year, then multiplying the result by 100. This graph is scaled to demonstrate the change in the percentage of the population represented by students reported under the category of autism.
In 2020, the Department started requiring states to report their 5-year-old kindergartners in school age educational environments. As a result of this shift in data collection for 5-year-olds, this figure presents data for the 5-year-old school age populations as two new trend lines beginning in 2020. The new trend lines are represented by a diamond symbol for ages 5 (school age) through 11 and a square symbol for ages 5 (school age) through 21. In this figure, the trend lines for ages 6 through 11 and ages 6 through 21 end in 2019.
Environmental Protection Agency (EPA)
EPA’s America’s Children and the Environment (ACE) Report was first initiated by EPA in 2000 and brings together environmental, biomonitoring, and health data from a variety of sources to provide national-level indicator data and related information on the environment and children’s health. ACE Report indicators is to better understand the impact environmental hazards have on children and educate policymakers, state and local environmental health partners, and the public on trends and areas that need further attention.
For the ACE Report, EPA analyzes and summarizes autism prevalence data from children ages 5 to 17, including survey data first collected in 1997 through 2019. Data for the autism indicator are obtained from an annual survey conducted by the CDC’s NCHS. The survey consists of a parent or other knowledgeable adult in each sampled household being asked questions regarding the child’s health status, including if they have ever been told the child has autism. From 2011 to 2013, the term "autism" in the survey was revised to "autism/autism spectrum disorder." Beginning in 2014, the term "autism" in the survey was revised to "autism, Asperger's disorder, pervasive developmental disorder, or autism spectrum disorder." EPA’s review and summary of the autism indicator, as part of the ACE Report, provides more details.
From 1997 to 2013, the percentage of children ages 5 to 17 years reported to have ever been diagnosed with autism rose from 0.1% to 1.2%. This increasing trend is statistically significant. Between 2014 and 2019, the rates of reported autism ranged from 2.3% to 2.9%. The higher reported percentages in these years might be due in part to the recent broadening of the definition of autism used in the survey question, as discussed above. Figure 2 provides an overview of autism prevalence over time, based on data obtained from NCHS.
Since 1999, the percentage of children reported to have autism in the United States has increased by 12-fold. For the year 2019, the rates of autism reported were approximately 3.3 times higher for boys than in girls, at 4.4% and 1.3%, respectively. This difference is statistically significant. Puerto Rican children (4.6%) had the highest rates of autism, followed by American Indian and Alaska Native children (3.8%), White children (2.9%), Black children (2.7%), Hispanic children (2.3%), Mexican children (2%), and Asian children (1.7%). The prevalence of autism in 2019 was similar for children living below the poverty level (2.8%) and those living at or above the poverty level (2.6%).
Figure 2. Prevalence rates of autism by gender, from 1997 to 2019.
Data for the autism indicator are obtained from an ongoing annual survey conducted by the NCHS.
* In 2014, the term "autism" in the survey was revised to "autism, Asperger’s disorder, pervasive developmental disorder, or autism spectrum disorder."
Average Age of Diagnosis
This portion of the report covers Section 399DD(a)(2)(D) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which requires: (D) "Information on the average age of diagnosis for children with autism spectrum disorder and other disabilities, including how that age may have changed over the 4-year period beginning on September 30, 2019, and, as appropriate, how this age varies across population subgroups." Information on the average age of diagnosis for individuals with ASD is provided by HHS’s CDC.
HHS Centers for Disease Control and Prevention (CDC)
Most children who have ASD are not diagnosed until after they reach 4 years of age, even though many children can be identified before 2 years of age. For the most recent ADDM Network ASD prevalence study from the CDC published in 2023, the median age of earliest known diagnosis was 49 months. Diagnosis is consistently earlier for children with ASD and co-occurring intellectual disability, with a median age of 43 months compared to 53 months for children with ASD without intellectual disability.
Many articles point to lack of change in the median age of diagnosis over years as an indication that there has not been progress in early identification of autism. However, median age metrics have substantial limitations that can mask progress. CDC published a paper comparing median age of identification to other metrics and found that an alternative measure, cumulative incidence of diagnosis (i.e., the number of children with an ASD diagnosis or special education eligibility at or before each month of age divided by the total population), better reflected progress in early identification over time, with more than four times as many children identified by age 48 months in 2016 than in 2002.58 This measure also revealed striking disparities in early identification by race and cognitive ability. Black and Hispanic children without intellectual disability were 30% less likely to be identified with ASD than White children, but Black children were 50% more likely than White children to be identified with ASD and intellectual disability. CDC is now using cumulative incidence of identification for surveillance of progress in early identification. Since 2016, comparisons with children aged 8 years have shown more early identification of ASD by age 48 months among younger cohorts. In surveillance year 2020, children born in 2016 (4-year-olds) were 1.6 times as likely as children born in 2012 (8-year-olds) to be identified as having ASD by 48 months of age. These patterns likely indicate improvements in practices among families, health care providers, and educators to evaluate and identify children with ASD early.
For the 2020 surveillance year, CDC analyzed incidence of ASD identification (earliest diagnosis or eligibility) by calendar month to quantify the impact of the COVID-19 pandemic. Identification among 4- and 8-year-old children was compared during the first four years of life. Prior to the COVID-19 pandemic there were large increases in early autism detection among the children who were 4 in 2020. After the pandemic began in March of 2020, progress in early autism detection was disrupted. Compared to what 8-year-olds experienced four years previously, the 4-year-olds had significantly less autism identification, and there was not recovery to pre-pandemic levels by the end of 2020. Disruptions in timely evaluation of children during the pandemic could have long-lasting effects as a result of delays in the identification and initiation of services during this unprecedented time.
In addition to collecting age of diagnosis data through ADDM, CDC’s Learn the Signs. Act Early. program provides parents, childcare professionals, and health care providers with free resources, in English, Spanish, and other languages, for monitoring children’s development. The program offers parent-friendly, research-based milestone checklists for children as young as 2 months of age. The Milestone Tracker app can help parents track their child’s development and take action to identify early developmental concerns so that children and families can get the services and support they may need at the earliest age possible.
Average Age of Intervention
This portion of the report covers Section 399DD(a)(2)(E) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which requires: (E) "Information on the average age for intervention for individuals diagnosed with autism spectrum disorder and other developmental disabilities, including how that age may have changed over the 4-year period beginning on September 30, 2019, and, as appropriate, how this age varies across population subgroups." Information on the average age of intervention for individuals with ASD is provided by HHS’s ACF and CDC.
HHS Administration for Children and Families (ACF)
ACF’s OHS administers grant funding and oversight to the 1,600 agencies that provide Head Start services in communities across the country. Children who attend Head Start programs range in age from birth to the age of school eligibility (5 years old). Head Start children identified with and receiving services for autism are therefore less than 5 years old. The number of preschool children with autism served by Head Start from 2019-2023 is listed in Table 18. It should be noted that there is no specific data about the timing of diagnosis of Head Start children from birth to 5 with IFSPs.
Table 18: Number of preschool children with autism served by Head Start from 2019-2023.
| Number of Preschool Children with Autism Served by Head Start: 2019 – 2023 | |
|---|---|
| Year | Number of Preschool Children with Autism |
Year2019 |
Number of Preschool Children with Autism4,195 |
Year2020 |
Number of Preschool Children with AutismN/A* |
Year2021 |
Number of Preschool Children with Autism3,536** |
Year2022 |
Number of Preschool Children with Autism4,996 |
Year2023 |
Number of Preschool Children with Autism6,661 |
* No data was collected for 2020 due to disruptions caused by the COVID-19 pandemic.
** Enrollment in 2021 was reduced due to the COVID-19 pandemic.
HHS Centers for Disease Control and Prevention (CDC)
Increasing access to additional data sources, such as Medicaid and IDEA, Part C, early intervention data, continues to be a goal of the ADDM Network’s early identification work in order to improve the capacity of the ADDM Network to estimate age at intervention. In 2020, the ADDM Network included more data sources than ever before. All 11 ADDM sites had access to records from medical service providers that evaluated children with developmental disabilities. Nine of the 11 ADDM sites had data agreements in place with education sources covering 100% of their study areas; Missouri had agreements with education data sources covering 50.3% of its study area, and Georgia had agreements with education data sources covering 97.6% of its study area. Maryland, Utah, and Wisconsin had access to IDEA, Part C, early intervention data. Arizona, California, and Wisconsin also had access to state-funded services such as Medicaid or disability services programs.
Data from upstream steps, including screening and referrals, could help identify inequities or barriers to services. Because the COVID-19 pandemic began part way through the surveillance year (2020), future surveillance years could reveal the magnitude and persistence of COVID-19 pandemic effects on ASD identification in communities. Additionally, because earlier identification could lead to better outcomes, follow-up of children suspected but not confirmed of having ASD could help minimize delays in identification and intervention.
Average Time Between Screening, Diagnosis, and Intervention
This portion of the report covers Section 399DD(a)(2)(F) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which requires: (F) "Information on the average time between initial screening and then diagnosis or rule out for individuals with autism spectrum disorder or other developmental disabilities, as well as information on the average time between diagnosis and evidence-based intervention for individuals with autism spectrum disorder or other developmental disabilities and, as appropriate, on how such average time varies across population subgroups." Information on age at first developmental evaluation and ASD diagnosis or special education eligibility is provided by HHS’s CDC.
HHS Centers for Disease Control and Prevention (CDC)
CDC’s ADDM Network findings on age of diagnosis of ASD support CDC’s Learn the Signs. Act Early. program, which aims to improve early identification by promoting early childhood developmental monitoring by parents, childcare providers, and health care providers. CDC continues to track the number and characteristics of children with ASD while also working to understand factors associated with outcomes among children and adolescents with ASD as they age and transition to adulthood.
Tracking the age at first developmental evaluation is important because services can begin immediately to address the specific impairments identified in a comprehensive evaluation, even before a diagnosis of ASD is made. Among 4-year-old children with ASD with a developmental evaluation, 78% were evaluated by age 36 months, with variability across sites ranging from 66.7% in Tennessee to 87.8% in Arkansas, based on ADDM data collected in 2020.3 Evaluation by age 36 months was similar by sex and by racial and ethnic groups, except for being lower among Black (75.9%) compared with Hispanic (79.8%) children. Similar percentages of children with and without co-occurring intellectual disability were evaluated by age 36 months (82.4% and 85.1%, respectively), but the percentage was lower among children without intellectual ability information (68.5%). For comparison, in 2018, 72% of 4-year-old children identified with ASD with a developmental evaluation were evaluated by age 36 months.12
Prevalence of ASD among children aged 4 years increased 26%, from 17.0 per 1,000 children in 2018 to 21.5 in 2020. However, prevalence varied widely across sites in 2020, with prevalence 265% higher in California than in Utah, the site with the lowest prevalence. This likely reflects community factors influencing early ASD identification. California continued to report high levels of early ASD identification, with higher prevalence at age 4 years than 8 years in 2020. Local factors likely contribute to early identification at the California site, such as hundreds of pediatricians participating in the Get SET Early model, which was supported by funding from the NIH (R01MH104446), and a state-funded regional center that provides evaluations and service coordination for persons with disabilities and their families. Variability in state-level procedures for early intervention also could contribute to differences in prevalence among sites. For example, in Maryland, early intervention is embedded within the school system, the health department, or shared between both (and other agencies such as social services). Such variability is likely seen across states and can potentially lead to different paths to accessing services.
Effectiveness and Outcomes of Interventions
This portion of the report covers Section 399DD(a)(2)(G) and (H) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which require: (G) "Information on the effectiveness and outcomes of interventions for individuals diagnosed with autism spectrum disorder, including by severity level as practicable, and other developmental disabilities and how the age of the individual or other factors, such as demographic characteristics, may affect such effectiveness" and (H) "Information on the effectiveness and outcomes of innovative and newly developed intervention strategies for individuals with autism spectrum disorder or other developmental disabilities." Information on funded projects and research findings that address the effectiveness and outcomes of interventions is provided by HHS’s ACL, AHRQ, HRSA, NIH, and SAMHSA, as well as DoD and ED.
Department of Health and Human Services (HHS)
Administration for Community Living (ACL)
ACL NIDILRR’s research and development portfolio from FY 2018 to FY 2023 has focused on the development of interventions to improve outcomes for individuals with disabilities such as ASD, including community living and participation among children with autism, education (primarily postsecondary education) and employment among transition age youth and adults with autism, and community living and participation among transition age youth and adults with autism. The following grants either focus exclusively on autism or include people with autism in their populations of interest.
Interventions
Parents Taking Action eHealth Adaptation and Pilot for Latinx, Black, and Chinese Families of Young Children with Autism Spectrum Disorder (90IFST0008; University of Illinois)
The objectives of this project are to adapt three culturally tailored versions of Parent Taking Action for Black (in English), Latinx (in Spanish), and Chinese (in Simplified Chinese) families into bite-sized online learning content and to evaluate the feasibility, acceptability, and preliminary evidence of efficacy of the adapted intervention. In the pilot phase, both family and child outcomes are evaluated using both observational data and standardized measures.
SAFE Program: Development and Refinement of a Peer Support Intervention for the Prevention of Infectious Airborne Diseases in the Workplace for Individuals with Autism Spectrum Disorders (90IFDV0023; Temple University)
This project develops and refines the SAFE program, an accessible peer support program to ensure safety and prevention of infectious airborne diseases for adolescents and young adults (ages 16-27 years) with ASD receiving employment services.
The Online and Applied System for Intervention Skills (OASIS) – Scaling-Up! (90DPKT0003; University of Kansas Medical Center)
This project follows standard implementation guidelines to scale-up Online and Applied Systems Intervention Skills (OASIS) to the broader community. OASIS is a program that uses a Research-to-Practice Outreach Training model to teach parents of children with ASD how to implement empirically based interventions with their children.
Further Development, Refinement, and Evaluation of the Online and Applied System for Intervention Skills Learning Management System (90BISB0025; Behavioral Technologies Consulting Organization, Inc.)
The overall goal of this project is to fully develop and test the Online and Applied System for Intervention Skills – Supervision, an online platform designed to build professional capacity for individuals pursuing the Board-Certified Behavior Analyst credential to primarily to serve individuals impacted by ASD. During this phase, this project develops and integrates a within-system video review feature to ensure HIPAA (Health Insurance Portability and Accountability Act of 1996)/FERPA (Family Educational Rights and Privacy Act) compliance, expands the content to match the current professional supervision requirements, and fully develops/deploys the supervision hours tracking feature.
Efficacy of the ASD Screening and Parent Engagement Intervention Program in Low-Resource Communities (90IFST0004; Texas State University)
The goal of this project is to examine the efficacy of the ASD Screening and Parent Engagement intervention, a culturally informed parent-mediated intervention program, when delivered to caregivers and children at risk for ASD who reside in low-resource households. The result is an intervention that is culturally and linguistically informed, acceptable and feasible in these communities, and leads to gains in social communication and reduction in challenging behavior in children at risk for ASD and gains in knowledge and skills for their parents and caregivers.
Rehabilitation Research and Training Center on Employment of People with Intellectual and Developmental Disabilities (90RTEM0003; Virginia Commonwealth University)
The Virginia Commonwealth University Rehabilitation Research and Training Center on Employment of People with Intellectual and Developmental Disabilities provides needed information in employer practices that are associated with better employment outcomes for individuals with intellectual and developmental disabilities. One project investigates how college students with ASD can use cognitive technology to impact their academic and employment outcomes.
Effects of Customized Employment on the Employment Outcomes of Transition-Age Youth with Disabilities: A Randomized Clinical Trial (90DP0085; Virginia Commonwealth University)
This project researches the use of customized employment as an intervention to assist individuals with intellectual disabilities and/or ASD to achieve and improve integrated employment outcomes.
Enhancing Community Participation for Adults with Autism Spectrum Disorders Through Peer-Mediated Transportation Interventions (90IFRE0013; Temple University)
This project developed and tested a peer-mediated intervention to reduce barriers to public transportation for transition age youth and adults with ASD. Transportation is a major obstacle to accessing essential services and overall community participation for many individuals with ASD. The goals of this project were to: (1) implement a randomized control study with 64 participants to determine the efficacy of an innovative peer-mediated intervention to reduce transportation barriers for transition age youth and adults with ASD; (2) determine dosing recommendations for the intervention; and (3) collect qualitative data to identify potential outcomes for future studies targeting peer-interventionists.
Efficacy of a Community College Transition Program for Young Adults with Autism Spectrum Disorder (90IFRE0019; University of North Carolina at Chapel Hill)
The goal of this project is to assess the feasibility, social validity, and efficacy of the Treatment and Education of Autistic and Related Communication Handicapped Children (TEACCH) School Transition to Employment and Postsecondary Education Program (T-STEP) intervention for 16- to 21-year-old community college students with ASD. The objectives of this 3-year study are (1) to conduct a pilot study including key stakeholder feedback to refine the T-STEP to ensure social validity and feasibility in a community college setting; (2) to examine the efficacy of the T-STEP in both in-person and online formats (with 45 young adults with ASD receiving the intervention and 45 young adults in a waitlist control group); (3) to examine characteristics of adults who most benefit from the program; and (4) to describe employment and college outcomes three months after program completion.
Exploratory Research
Using GIS and GPS Techniques to Understand Meaningful Participation for Adults with Autism Spectrum Disorder (90SFGE0008; University of North Carolina School of Medicine)
The purpose of this study is to use innovative Global Positioning System (GPS) and Geographic Information System (GIS) measures to systematically assess the community participation of adults with ASD and investigate critical environmental and personal factors associated with participation. The primary goal of this project is to advance the understanding of where and how adults with ASD spend their time, how they interact with their community, and what resources or supports promote community participation.
Small Business Innovation Research (SBIR)
SkillTalk: Using Streaming Video for Young Adults with Autism Spectrum Disorder to Build Microskills to Develop and Sustain Relationships for Healthy and Independent Living (Phases I and II) (90BISA0037 and 90BISB0022; dfusion, Inc.)
Phase I of this project developed and tested SkillTalk, a prototype video-delivered microskills training program to improve relationship skills among transition age adults with ASD between 18 and 28 years of age. Microskills such as showing empathy, active listening, and open-ended questioning can help build relationships. The Phase II project will complete the development and evaluation of SkillTalk.
Summer Job Story for Transition Age Youth Who Have Autism Spectrum Disorder and are Considered High Functioning (90BISA0055; Objective Ed, Inc.)
The goal of this project is to determine the feasibility of using an Animated Spoken Interactive Fiction story to help young high school high functioning students with ASD between 14- and 16-years old practice pre-employment transition skills to obtain a summer job and to provide information to teachers so they may deliver more targeted instruction and better utilize instructional time.
Leveraging Self-Management Technology to Augment Social Skills for Employment for Individuals with Autism (90BISA0061; Cognitopia)
This project develops and evaluates a prototype of the System to Augment Social Skills for Employment, designed to augment self-management and training in social skills for individuals with autism and the employment professionals who support them, with the goal of better long-term sustained employment.
Agency for Healthcare Research and Quality (AHRQ)
Research projects funded by AHRQ in FY 2019 – FY 2023 that seek to develop new and improve the effectiveness of existing interventions for individuals with autism are described below.
The interplay of behavioral therapies, pharmacological treatments and psychiatric adverse events among Youth with Autism Spectrum Disorder (R01HS029003; Pennsylvania State University)
Understanding treatment utilization patterns and variations across demographic, geographic, and socioeconomic factors will provide guidance to improve the efficiency of health care delivery and quality of health services for individuals with ASD. Leveraging large, national, longitudinally constructed Medicaid claims databases (2008-2022), this project will examine the interplay between polypharmacy of psychotropic medications and key ASD behavioral therapies among youth aged 5-26 with ASD and evaluate their impact on preventing behavioral health crises. The study will provide a comprehensive assessment of the quality of ASD-related treatments and services in a real-world setting and shed light on disparities in service use, quality of care, and health outcomes, particularly in regard to the risk of behavioral health crises among youth with ASD. This information will be valuable to families exploring treatment options, as well as to providers in determining treatment options to maximize benefit. Identifying barriers to accessing services and implementation of evidence-based practice will help guide policies at the payer, state, and national levels.
Ambulatory Pediatric Safety Learning Lab (R18HS026644; Boston Children’s Hospital)
Approximately 40% of children with ASD take anti-psychotic medications, and most are not screened for complications. One of the aims of the Ambulatory Pediatric Patient Safety Learning Lab is to study children with ASD on antipsychotic medication to create processes for patient/family medication monitoring and communication with clinics to prevent adverse drug events. Additionally, the project aims to design a workflow to plan for, detect, and prompt management of serious illness among children with chronic conditions, including children with ASD, at home. The overarching goal is to redesign systems of care and coordination between the clinic and home to eliminate harm due to health care in these settings. Problem analysis will include ethnography in the home and clinic, interviews, Failure Mode and Effects Analysis, and digital diaries. The researchers will implement all interventions together in the simulated environment and evaluate using a randomized factorial trial, followed by implementation in the clinical system with qualitative and quantitative evaluation. The intent is to develop a scalable model which leverages health systems and patient/family strengths to ensure safe health care among all children. Upon completion of this proposal, the research team aims to scale this nationally through the Solutions for Patient Safety Network and improve pediatric ambulatory safety across the United States.
Understanding Early Intervention Value: Investigating the Effect of a Statewide Care Coordination Model on EI Resource Use and Outcomes (R01HS027583; University of Colorado Denver)
Infants and toddlers with developmental delays and disabilities often receive IDEA, Part C, Early Intervention (EI) to improve function. This project seeks to characterize EI family-centered care coordination (FC-CC) and understand how FC-CC practices relate to value-based EI: better outcomes at lower cost. First, this project seeks to understand the effect of a statewide EI FC-CC model called Global Outcomes for Infants and Toddlers (GO4IT). GO4IT integrates family assessment, care planning processes, outcomes measurement with the goal of identifying salient family needs, individualizing service type and intensity, and improving global measures of child function. This quantitative analysis will use state EI administrative databases for Colorado and Massachusetts and is in the context of state-wide implementation of GO4IT, which provide an "exogenous shock" to value-based EI service delivery that allows for the examination of changes in EI service use and outcomes before and after GO4IT. Second, researchers will conduct about 30 interviews with EI stakeholders to determine FC-CC mechanisms, successes, and best practices. GO4IT is one example of a service delivery package designed to best meet the needs of families while also providing information for families and EI providers to promote family engagement in care planning and optimal outcomes. This study will provide evidence to inform future efforts to implement FC-CC programs. The proposal aligns with AHRQ's funding priorities of value-based care, includes the priority population of children with special health care needs, and aligns with the Health Services Research Priorities for Achieving a High Value Healthcare System (NOT-HS-19-011) with a focus on children ages 0-3.
Health Resources and Services Administration (HRSA)
HRSA’s research programs conduct a range of studies that focus on how factors, such as severity level, age of child, and demographic characters, may affect the effectiveness of interventions for individuals diagnosed with autism and developmental disabilities. HRSA research programs additionally conduct a range of studies on innovative interventions and newly developed intervention strategies for individuals with ASD and other developmental disabilities. A selection of noteworthy studies is described below.
Autism FIRST studies have evaluated modified interventions that address barriers to intervention effectiveness across various contexts, including with minimally verbal children, among racial/ethnic minorities, and in disadvantaged geographic locations and contexts. For example, one FIRST study was effective in lowering stress level and improving caregiver skills, while also improving engagement, play frequency, and joint attention behaviors in toddlers. Autism FIRST studies also conduct and test innovative interventions across study settings, developmental stages, and subpopulations. The studies have focused on a broad range of topics to include telehealth parent training, mindfulness training to enhance parent-coaching, teacher-mediated toilet training using a manualized moisture alarm, and training parents to implement ABA.
Autism secondary analysis studies in SDAR have identified barriers to early intervention such as measurement bias in diagnostic tools and the impact of adverse family experiences of underrepresented minorities on seeking services (i.e., children with ASD experience more adverse childhood experiences, including neighborhood violence, parental divorce, parental mental illness, and parental substance abuse). Research is addressing disparities in early identification of ASD and subsequent service utilization. One study demonstrated the effectiveness of an evidence-based screening program and evidence-based training protocols for primary care staff that was adapted for use with Latino families. This early screening intervention increased the rate of completion of the Modified Checklist for Autism in Toddlers (M-CHAT), a standardized developmental tool for eligible children ages 18 and 24 months, from less than 5% prior to the onset of the intervention to approximately 60% after three months of implementation and nearly 100% at six months.
Project EARLY, conducted by DBPNet, evaluated an individually tailored, culturally informed family navigation intervention to improve access to ASD diagnostic and treatment services (including early intervention services) and outcomes for children who screen positive for ASD at pediatric primary care centers serving low-income communities. Study results support the conclusion that family navigation improved the likelihood of ASD diagnosis among children from racial/ethnic minority, low-income families at risk of ASD and identified a new method to evaluate family navigation implementation, with a focus on early detection and mitigation of failures in the process.
DBPNet additionally conducted a study examining the consistency between a developmental behavioral pediatrician’s diagnostic impression (ASD or not ASD) prior to administration of the Autism Diagnostic Observation Schedule (ADOS) and then again after the ADOS was administered. This study found that clinical diagnoses of autism were consistent with the ADOS in 90% of cases. Further analysis suggests that the ADOS is often not required for ASD diagnosis by DBPs and that DBPs can identify children for whom the ADOS may be helpful. As ASD diagnostic assessments that do not include the ADOS are less time consuming and costly, study findings indicate that streamlined assessments could improve access to timely diagnosis and reduce barriers to intervention and treatment.
AIR-B studies focus on developing and testing the efficacy of behavioral interventions for children with ASD in school and community-based settings. Results from the multi-site, formative research phase of AIR-B’s Mind the Gap study found that the best place to intervene was with families waiting to receive services. Informed by the formative research with parents and providers of low-income, minority children with ASD, the ongoing Mind the Gap intervention is a community-driven intervention for low-income parents and minority children with ASD that is low intensity and likely to be both effective and sustainable, resulting in increased access to care for under-resourced children.
Another AIR-B study examined autistic and non-autistic college students’ experiences of discrimination and harassment and identified protective and risk factors. Findings highlighted the importance of faculty support in fostering positive interpersonal experiences on campus and demonstrated the need to address deeper college campus issues with respect to neurodiversity. AIR-B is currently studying implementation strategies for three interventions using the UNITED (Using Novel Implementation Tools for Evidence-based intervention Delivery) framework.
The AIR-P implements research studies examining factors such as diagnosis and treatment of co-morbidities to improve outcomes in individuals receiving treatment for ASD. One study found that a fixed dose of metformin can be effective for decreasing weight gain associated with atypical antipsychotic medication used to treat ASD in children and adolescents.
HWRN studies examine feeding and weight management in children and adolescents diagnosed with ASD. One study is evaluating the impact, acceptability, and feasibility of a pilot adaptive weight management intervention for overweight children with ASD aged 4 to 8 years old.
ALDP conducted the first prospective study to show temporal and dose-response associations of cord blood biomarkers of acetaminophen with increased risk of developing autism and ADHD. This study addressed major methodological issues identified by the FDA, American Academy of Pediatrics, and others. This led to updated advice to pregnant women regarding acetaminophen during pregnancy.
The ATRP study investigating health inequities faced as autistic individuals age into adulthood found heightened risk for developing diabetes, cardiovascular diseases, and hypertension within marginalized groups. The study highlights the need for improved prevention and screening for these conditions and the provision of supports to improve health outcomes.
National Institutes of Health (NIH)
NIH supports research to develop, test, and improve high-quality, evidence-based interventions and services to maximize health and well-being for all people with ASD and their families.
- NICHD-supported researchers focused on the development of a telehealth screener and assessment for infants at risk for ASD. The researchers concluded that screening should begin early, and be repeated, but that there is not one "best" schedule for autism screening (PMID: 33711288).59 Both screening and developmental surveillance are needed to identify as many toddlers with ASD as possible.
- Researchers supported by NICHD, NIEHS, and NIMH found that children with ASD scored higher for sleep problems at 6 and 12 months compared to the other groups. These children also had more growth in the brain’s hippocampus region from 6 to 24 months compared to children without sleep problems (PMID: 32375538).60
- NIMH-supported researchers found that early screening in universal and targeted settings increases early access to autism services and may be particularly beneficial for families from historically marginalized populations (PMID: 33427861; PMID: 34982099).61,62
- NICHD- and NIMH-funded researchers evaluated potential early correlates of autism documented in electronic health records (EHRs) during routine care that could improve accuracy of early ASD detection. The researchers used EHR data to train an early autism detection model (a computer algorithm) that could predict a later autism diagnosis with clinically meaningful accuracy with records starting at 1 month of age. The model’s accuracy improved when using records from children at older ages (PMID: 36729455).63
- NICHD- and NCATS-supported researchers investigated the utility of a mobile app that enables caregivers to collect data on behaviors of children with ASD and to help identify children that would benefit from referral for additional testing. This tool, which uses computer vision to capture and analyze a child’s behavior while the child watches a video on a tablet, could assist in detecting signs of atypical social development and reduced attention in toddlers with ASD (PMID: 29595333).64
- NICHD-supported researchers are assessing an approach to help children ages 3 to 4 with ASD who are at high risk for being minimally verbal by age 6 and will examine how best to augment interventions for children who respond slowly to initial interventions (R01HD095973).
- NICHD-supported researchers adapted a community-based intervention for improving social communication in children with ASD to include peer participation. Children who participated in the intervention made gains in social communication and play skills, and they were more engaged with peers when adults were present (PMID: 32643385).65
- NICHD-, NIMH-, and NIDCD-supported researchers aimed to develop methods for predicting intervention response in order to better personalize early interventions. Researchers provided an intervention to children ages 3 to 5 who used limited spoken language to communicate and found that the ability to play appropriately with a wider variety of toys best predicted improvements in expressive language following the intervention (PMID: 35437928).66
- NICHD-, NIBIB-, and NIGMS-supported researchers designed an AI-driven wearable behavioral intervention to encourage facial engagement (use of facial expressions in social interactions) and provide social feedback to children with ASD. Children used the intervention at home over six weeks, and researchers assessed socialization in the clinic. Children who participated in the intervention with concurrent ABA therapy showed improved emotion recognition and facial engagement (PMID: 30907929).67
- NICHD-supported researchers developed a measure of social communication for describing baseline levels of social ability and subsequent changes in children with ASD. Researchers assessed data from three widely used autism symptom measures to identify four factors to model social communication, including basic skills, interaction quality, behavioral modification, and social initiation and affiliation. These factors may improve conceptual models of social communication, including mapping how deficits unfold in ASD versus other disorders (PMID: 33027686).68
- NIMH-supported researchers designed the Stepped Transition in Education Program for Students with ASD (STEPS) to prepare students with autism for the transition to postsecondary education. The researchers found that STEPS increased participants’ college readiness and decreased depressive symptoms over the transition period (PMID: 31609666).69
- NIMH-supported researchers developed an intervention to increase social engagement at work and school among young adults with autism, increase family capacity for accessing services, and improve adult outcomes. Participants enrolled in the intervention reported improvements in engagement in work-related activities and other meaningful activities and decreased problems with internalizing behavior (e.g., hurtful to self, unusual or repetitive habits, inattentive behavior; PMID: 34625016).70
- NIMH-supported researchers developed and tested a parent advocacy training program aimed at enabling parents’ efforts to advocate for continued services for their children as they transition into adulthood. Parents who completed the program reported that they learned more about the adult service system and were more skilled in advocating for their children (PMID: 28070786).71
- NICHD-supported researchers are studying individual and combined effects of two evidence-based interventions in real world settings. One approach engages families to access resources when they first learn their child has signs of ASD using an intervention with motivational interviewing and problem-solving education. The other approach coaches families to use social interaction intervention strategies for toddlers with ASD in everyday activities (R01HD093055).
- NIDCD- and NICHD-supported investigators developed an intervention for nonverbal and minimally verbal preschoolers with ASD that taught preschoolers with ASD and peers without disabilities to use speech-generating devices. Preschoolers with ASD in peer-mediated groups demonstrated increased rates of communication and reciprocity compared to children with ASD who had not learned to use speech-generating devices (PMID: 30054629).72
- NICHD-supported researchers used sensory integration therapy to improve functional skills in children with ASD and sensory issues. Researchers identified sensory difficulties that are not typically assessed or considered for individuals with ASD, and further research could lead to personalized treatments (PMID: 36167886).73
- NICHD- and NIA-supported researchers investigated changes in service needs and services received before, during, and after high school for people with ASD. People with ASD received fewer services as they transitioned out of high school, and these decreases were greater for those who had ASD and intellectual disability than it was for those who only had ASD (PMID: 31033222).74
NICHD- and NIMH-supported researchers examined the behavioral and social factors in early childhood that contribute to positive and negative outcomes in adults with ASD. In this longitudinal study, researchers analyzed the stability of autism diagnoses from early childhood through young adulthood and found that autism symptoms can change across development and are associated with gradual shifts in core features of autism beginning in childhood (PMID: 34890046).75
Substance Abuse and Mental Health Services Administration (SAMHSA)
While SAMHSA does not have autism-specific programs, SAMHSA programs may support those with ASD who may also have behavioral health conditions, and SAMHSA grantees are required to complete a disparity impact statement concerning the demographic characteristics of those served. It is important to note that individuals diagnosed with ASD need varying levels of support and not all individuals on the autism spectrum are labeled as having SED, SMI, and/or SUD.
SAMHSA collaborates with ACL, CMS, HRSA, and other agencies to support strategies to assist those with developmental disabilities, including those on the autism spectrum, and co-occurring behavioral health conditions. SAMHSA has also supported peer-reviewed publications and meetings to discuss how children with intellectual and developmental disabilities are treated within the behavioral health system and strategies to promote success. This included a roundtable discussion and issue brief developed by the National Association of State Mental Health Program Directors, National Association of State Directors of Developmental Disabilities Services, and National Association for the Dually Diagnosed, as well as two articles published in the journal Psychiatric Services.76,77 SAMHSA’s MHTTC Network has supported training on developmental disabilities and behavioral health conditions, and SAMHSA is also collaborating with ACL on a new center launched in 2022 to support programs for those with both developmental disabilities and behavioral health conditions.
Department of Defense (DOD)
Army
The DoD ARP invests heavily on research aimed at having an immediate impact on those with ASD, including research on effective and innovative intervention strategies. Examples of projects funded in FY 2019 – FY 2023 are described below.
- University of Missouri researchers are conducting an intervention study utilizing cognitive behavioral treatment for childhood insomnia (CBT-CI). This intervention will be delivered both in-person and remotely to school-aged children with autism and insomnia. The study seeks to determine if the CBT-CI intervention will improve the children’s sleep and daytime behavior and decrease the levels of arousal. Additionally, it is anticipated that there will be improvements in the parents’ sleep, arousal, mood, levels of fatigue, and stress. The goal of this work is to impact autism patient care through the development of a new treatment option for insomnia in school-aged children with ASD, which does not currently exist.
- Investigators at the Southwest Autism Research and Resource Center are testing a personalized, multi-faceted behavioral intervention, PEERS-plus. A group of adults with autism, aged 21-70, and their support companions will identify their individual needs for developing and maintaining functional independence. This intervention will then be used to address these key concerns for all ages by adding cognitive compensation training, mindfulness-based emotional regulation, and support group components to the well-established PEERS (Program for the Education and Enrichment of Relational Skills) social skills training program with the goal of improving independence and quality of life in adults with ASD.
- Researchers at the University of Colorado Denver are adapting the CBT manualized intervention Facing Your Fears. The intervention will be provided to adolescents with ASD and intellectual disability to test whether it is more effective in reducing anxiety than treatment-as-usual. Findings from this study would represent the first randomized clinical trial of a CBT intervention for adolescents with ASD/intellectual disability, a critical step toward establishing an evidence base for anxiety treatment for this underserved and vulnerable population.
- Cincinnati Children’s Hospital researchers developed Regulating Together (RT), an intensive outpatient group program addressing emotion dysregulation in youth with ASD. Emotion dysregulation has been linked to higher rates of psychiatric hospitalizations, suicidal ideation, school disciplinary action, rejection by peers, failed transition to college and employment, co-occurring psychiatric diagnoses, and use of psychotropic medications in individuals with ASD. This study will evaluate short-term and long-term efficacy and long-term functional outcomes of RT compared to a control intervention. Additionally, the team will examine facilitators and barriers to treatment response and implementation to guide future implementation and dissemination research of RT.
- Investigators at Hugo W. Moser Research Institute at Kennedy Krieger are examining the efficacy of a novel telehealth CBT intervention, DINO Strategies for Anxiety and Intolerance of Uncertainty Reduction (DINOSAUR), as a potential anxiety treatment in autistic children. This intervention targets both anxiety and intolerance of uncertainty in young autistic children. The objective of this study is to develop an efficacious anxiety treatment model for young autistic children with and without developmental delays. Treating anxiety when children with autism are young may produce a more robust treatment response. It may also improve outcomes by increasing children’s availability to engage in developmental interventions and by reducing long-term psychiatric risk.
- Researchers at Yale University are developing a novel intervention named Behavior Therapy for Irritability and Aggression (BTIA) for adolescents with ASD. BTIA includes structured, illustrated activities for teaching emotion regulation and problem-solving skills to the adolescent; a functional assessment to identify unique triggers of aggressive behavior; a parent component that teaches antecedent management and reward strategies; and a school component for disruptive behavior at school. The goals of BTIA are to help adolescents develop emotion regulation skills to handle frustration and to strengthen skills for navigating the challenging and diverse experiences associated with the transition to adulthood.
Military Health System (MHS)/TRICARE
The purpose of the ACD is to further analyze and evaluate the appropriateness of the ABA tiered-delivery model under TRICARE in light of current and anticipated certification board guidelines. The ACD seeks to establish appropriate provider qualifications for the proper diagnosis of ASD and for the provision of ABA services, assess the feasibility and advisability of establishing a beneficiary cost-share for ABA services for ASD, and develop more efficient and appropriate means of increasing access and delivery of ABA services under TRICARE while creating a viable economic model and maintaining administrative simplicity. The overarching goal of this demonstration is to analyze, evaluate, and compare the quality, efficiency, convenience, and cost-effectiveness of ABA services that do not constitute proven medical requirements that govern the TRICARE Program.
To acquire additional information on ABA services under TRICARE’s ACD, the DHA has been working with the Congressionally Directed Medical Research Program (CDMRP), which awarded a $7 million contract to a research group from the University of Rochester. The results of the CDMRP study will further the DHA’s understanding of the impact of ABA services delivered to ACD participants and aims to provide important data regarding the most beneficial amount of ABA services. Additionally, findings from this study may benefit the larger community of individuals diagnosed with ASD and their families in several ways, including, but not limited to, offering more choices to families, potentially identifying response to intervention through predictive factors, and lowering costs while increasing access. The CDMRP study was awarded September 2018. This study has provided annual reports to CDMRP beginning in 2020 and has a duration of five years.
TRICARE covers evidence-based treatment that is determined to be proven medical care as defined in statute and regulation. Only under the demonstration authority is the DHA authorized to cost-share ABA services. The DHA continues to monitor the autism research landscape to identify additional services and interventions that may demonstrate effectiveness for use in individuals diagnosed with ASD.
Department of Education (ED)
Institute of Education Sciences (IES)
IES’s NCSER funds a number of projects to develop and/or modify existing interventions intended to improve the educational and developmental outcomes of individuals on the autism spectrum. Through the Special Education Research Grants Program competition, NCSER has funded a number of projects that have demonstrated positive effects on children and youth with ASD. These projects are described below.
NCSER funded the development and testing of a framework for Supporting Early Interventionists of Toddlers with Autism to Build Family Capacity (R324A180083; Indiana University). This framework was designed to assist early intervention providers in implementing the Building Interactive Social Communication intervention. Providers used the intervention to help parents mediate social communication learning in toddlers with emerging signs of autism. Researchers used focus groups and an iterative development process to design a feasible and acceptable framework, and pilot tested the effects of the framework in 12 case studies in a multiple-baseline single-case design. The pilot study demonstrated a change in early interventionist practices, and a resulting increase in parents’ use of strategies to mediate social communication with their children. Effects on toddler behavior included improvements in social reciprocity, positive social behavior, joint attention, and symbolic play for 10 of the 12 participants.
NCSER funded work developing (R324A080136; State University of New York at Buffalo) and testing the efficacy of (R324A130216; Canisius College) a comprehensive school-based intervention (CSBI) for elementary school children with high-functioning ASD. This packaged intervention consisted of five components: social skills groups; therapeutic activities to promote the expansion of interests and to provide social practice; individual daily notes to prompt, practice, and reinforce newly learned skills; interactive computer instruction to teach recognition of emotions; and parent training to increase home-school communication. In an initial randomized controlled trial, researchers found that compared to children receiving typical instruction in control schools, children in CSBI schools demonstrated significantly better outcomes on measures of social cognition, social communication skills, and ASD symptoms. In a recently completed follow-up study (R324A180005; Canisius College), researchers demonstrated that these positive effects persisted one and a half years later, suggesting a durable impact of the intervention.
Additional projects funded by NCSER focused on developing and/or modifying existing interventions to improve the educational and developmental outcomes of children and youth with autism include:
- Betty’s Mind: A Theory of Mind and Social Reasoning Intervention for Adolescents with Autism Spectrum Disorders Based on a Learning by Teaching Approach (R324A180171; Vanderbilt University);
- Teaching Academic Success Skills to Middle School Students with Autism Spectrum Disorder (ASD) and Executive Functioning Deficits (R324A180053; Cincinnati Children’s Hospital Medical Center);
- Partnering with Early Intervention Providers to Increase Implementation of Parent Coaching for Families of Children with ASD (R324B180017; University of Pennsylvania);
- Teacher and Peer Speech in Inclusion Classrooms: Malleable Factors Affecting Language Outcomes for Children with Disabilities (R324A180203; University of Miami);
- Optimizing Emergent Literacy Interventions for Children with Autism (R324B180035; Florida State University);
- Efficacy of the Early Social Interaction (ESI) Model for Toddlers with Early Signs of Autism Spectrum Disorder in Community Early Intervention Programs (R324A180193; Florida State University); and
- Enhancing Peer Network Interventions to Improve Social Communication, Play, and Peer Relationships for Minimally Verbal Students with Autism (R324B210004; Vanderbilt University).
Office of Special Education and Rehabilitative Services (OSERS)
For purposes of this report, OSERS’ RSA analyzed data from the Case Service Report (RSA-911) (OMB Control #: 1820-0508) for Program Year (PY) 2018 through PY 2021. Although WIOA was signed into law on July 22, 2014, the WIOA performance accountability system requirements did not take effect until July 1, 2016. The data WIOA requires, as compared to data RSA included in the prior report, are fundamentally different. For example, prior to WIOA, state VR agencies collected and reported data only on those individuals who had exited the VR program. Under WIOA’s requirements, state VR agencies now must collect and report data on all program participants while they are still actively engaged with the program plus data on those who have exited the program. As another example, prior to WIOA, state VR agencies collected and reported data annually on a federal FY basis (October 1 through September 30). Under WIOA’s requirements, state VR agencies now report quarterly on a PY basis (July 1 through June 30). Given the scope and breadth of the data collection and reporting requirement changes resulting from WIOA, ED used the WIOA transition authority to give state VR agencies sufficient time to reconfigure their data collection systems. To that end, ED did not implement the WIOA data collection requirements until PY 2017, which began July 1, 2017. For purposes of this report, RSA has analyzed data covering PY 2018 through PY 2021 (July 1, 2018 – June 30, 2022).
RSA has provided the total number of individuals with autism as a primary or secondary cause of disability and the number of individuals whose primary disability was an intellectual disability. RSA also computed the average age at application for these individuals who were eligible for VR services.
Table 19: Number of individuals with autism as a primary or secondary cause of disability and the number of individuals with intellectual disability as the primary disability who were eligible for VR services in PY 2018 – PY 2021.
| Number of Individuals Eligible for VR: PY 2018 – PY 2021 | ||
|---|---|---|
| Program Year | Autism | Intellectual Disability |
Program Year2018 |
Autism38,575 |
intellectual Disability126,661 |
Program Year2019 |
Autism34,356 |
intellectual Disability103,317 |
Program Year2020 |
Autism29,422 |
intellectual Disability79,472 |
Program Year2021 |
Autism39,199 |
intellectual Disability101,871 |
Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
Table 20: Average age at application for individuals with autism as a primary or secondary cause of disability and individuals with intellectual disability as the primary disability who were eligible for VR services in PY 2018 – PY 2021.
| Average Age at Application for VR Services: PY 2018 – PY 2021 | ||
|---|---|---|
| Program Year | Autism | Intellectual Disability |
Program Year2018 |
Autism21.3 |
intellectual Disability23.98 |
Program Year2019 |
Autism21.47 |
intellectual Disability24.22 |
Program Year2020 |
Autism21.21 |
intellectual Disability23.71 |
Program Year2021 |
Autism21.35 |
intellectual Disability23.79 |
Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
RSA also analyzed the number of individuals with employment outcomes by age group, gender, and race/ethnicity for VR program participants (i.e., eligible individuals with disabilities who received VR services under an Individualized Plan for Employment [IPE]) whose primary or secondary cause of disability was reported as autism or whose primary disability was reported as intellectual disability.
Table 21: VR program participants with autism as a primary or secondary cause of disability and employment outcome by age at exit in PY 2018 – PY 2021.
| Number of VR Program Participants with Autism by Age at Exit: PY 2018 – PY 2021 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Program Year | <16 | 16-18 | 19-24 | 25-44 | 45-54 | 55-59 | 60+ | TOTAL |
Program Year2018 |
<160 |
16-18501 |
19-247,688 |
25-443,986 |
45-54212 |
55-5970 |
60+37 |
TOTAL12,494 |
Program Year2019 |
<160 |
16-18546 |
19-247,384 |
25-443,974 |
45-54194 |
55-5963 |
60+42 |
TOTAL12,203 |
Program Year2020 |
<160 |
16-18427 |
19-246,629 |
25-443,664 |
45-54175 |
55-5952 |
60+30 |
TOTAL10,977 |
Program Year2021 |
<160 |
16-18532 |
19-248,712 |
25-444,959 |
45-54211 |
55-5979 |
60+51 |
TOTAL14,544 |
Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
Table 22: VR program participants with intellectual disability as a primary cause of disability and employment outcome by age at exit in PY 2018 – PY 2021.
| Number of VR Program Participants with Intellectual Disability by Age at Exit: PY 2018 – PY 2021 | ||||||||
|---|---|---|---|---|---|---|---|---|
| Program Year | <16 | 16-18 | 19-24 | 25-44 | 45-54 | 55-59 | 60+ | TOTAL |
Program Year2018 |
<160 |
16-183,190 |
19-2424,708 |
25-4412,860 |
45-542,665 |
55-591,082 |
60+718 |
TOTAL45,223 |
Program Year2019 |
<162 |
16-182,669 |
19-2422,089 |
25-4411,652 |
45-542,106 |
55-59957 |
60+655 |
TOTAL40,130 |
Program Year2020 |
<161 |
16-182,119 |
19-2418,839 |
25-449,737 |
45-541,615 |
55-59627 |
60+500 |
TOTAL33,438 |
Program Year2021 |
<162 |
16-182,177 |
19-2420,682 |
25-4411,807 |
45-541,944 |
55-59754 |
60+658 |
TOTAL38,024 |
Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
Table 23: VR program participants with autism as a primary or secondary cause of disability and employment outcome by gender in PY 2018 – PY 2021.
| Number of VR Program Participants with Autism by Gender: PY 2018 – PY 2021 | ||
|---|---|---|
| Program Year | Male | Female |
Program Year2018 |
Male10,320 |
Female2,140 |
Program Year2019 |
Male10,178 |
Female1,987 |
Program Year2020 |
Male9,076 |
Female1,856 |
Program Year2021 |
Male11,881 |
Female2,587 |
Data excludes participants who did not identify their gender. Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
Table 24: VR program participants with intellectual disability as a primary cause of disability and employment outcome by gender in PY 2018 – PY 2021.
| Number of VR Program Participants with Intellectual Disability by Gender: PY 2018 – PY 2021 | ||
|---|---|---|
| Program Year | Male | Female |
Program Year2018 |
Male28,409 |
Female16,730 |
Program Year2019 |
Male25,156 |
Female14,895 |
Program Year2020 |
Male21,074 |
Female12,288 |
Program Year2021 |
Male23,628 |
Female14,254 |
Data excludes participants who did not identify their gender. Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
Table 25: VR program participants with autism as a primary or secondary cause of disability and employment outcome by race/ethnicity in PY 2018 – PY 2021.
| Number of VR Program Participants with Autism by Race/Ethnicity: PY 2018 – PY 2021 | ||||||
|---|---|---|---|---|---|---|
| Program Year | Race | Ethnicity: Hispanic or Latino | ||||
| White | Black or African American | American Indian or Alaska Native | Asian | Native Hawaiian or Other Pacific Islander | ||
Program Year2018 |
White10,718 |
Black or African American1,361 |
American Indian or Alaska Native193 |
Asian443 |
Native Hawaiian or Other Pacific Islander73 |
Ethnicity: Hispanic or Latino1,017 |
Program Year2019 |
White10,285 |
Black or African American1,474 |
American Indian or Alaska Native166 |
Asian457 |
Native Hawaiian or Other Pacific Islander69 |
Ethnicity: Hispanic or Latino1,027 |
Program Year2020 |
White9,305 |
Black or African American1,236 |
American Indian or Alaska Native162 |
Asian372 |
Native Hawaiian or Other Pacific Islander65 |
Ethnicity: Hispanic or Latino948 |
Program Year2021 |
White12,182 |
Black or African American1,749 |
American Indian or Alaska Native205 |
Asian540 |
Native Hawaiian or Other Pacific Islander78 |
Ethnicity: Hispanic or Latino1,398 |
More than one race/ethnicity may be reported for a participant. Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
Table 26: VR program participants with intellectual disability as a primary cause of disability and employment outcome by race/ethnicity PY 2018 – PY 2021.
| Number of VR Program Participants with Intellectual Disability by Race/Ethnicity: PY 2018 – PY 2021 | ||||||
|---|---|---|---|---|---|---|
| Program Year | Race | Ethnicity: Hispanic or Latino | ||||
| White | Black or African American | American Indian or Alaska Native | Asian | Native Hawaiian or Other Pacific Islander | ||
Program Year2018 |
White34,095 |
Black or African American9,820 |
American Indian or Alaska Native874 |
Asian979 |
Native Hawaiian or Other Pacific Islander254 |
Ethnicity: Hispanic or Latino7,270 |
Program Year2019 |
White29,781 |
Black or African American9,035 |
American Indian or Alaska Native780 |
Asian879 |
Native Hawaiian or Other Pacific Islander233 |
Ethnicity: Hispanic or Latino6,217 |
Program Year2020 |
White25,031 |
Black or African American7,292 |
American Indian or Alaska Native612 |
Asian723 |
Native Hawaiian or Other Pacific Islander176 |
Ethnicity: Hispanic or Latino5,489 |
Program Year2021 |
White28,553 |
Black or African American8,028 |
American Indian or Alaska Native691 |
Asian923 |
Native Hawaiian or Other Pacific Islander219 |
Ethnicity: Hispanic or Latino6,357 |
More than one race/ethnicity may be reported for a participant. Data for PY 2022 and PY 2023 were not available at the time this report was written.
Source: U.S. Department of Education: Office of Special Education and Rehabilitative Services: Rehabilitation Services Administration: Case Service Report (RSA-911).
Home- and Community-Based Services (HCBS) and Supports
This portion of the report covers Section 399DD(a)(2)(J) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which requires: (J) "Information on how States use home- and community-based services and other supports to ensure that individuals with autism spectrum disorder and other developmental disorders are living, working, and participating in their community."
HCBS are types of person-centered care delivered in the home and community. HCBS programs address the needs of people with functional limitations who need assistance with everyday activities, such as transferring out of bed, getting dressed, and bathing. HCBS are often designed to enable people to stay in their homes rather than moving to a facility for care. They also can support individuals residing in institutions, including individuals with autism, to transition to the community and receive long-term services and supports (LTSS) in the setting of their choice. Information on home- and community-based services and supports is provided by HHS’s ACL and CMS, as well as HUD and DOL.
Department of Health and Human Services
Administration for Community Living (ACL)
To make community living possible for millions of people with disabilities and older adults, ACL funds direct services and supports provided primarily through networks of community-based organizations; invests in training, education, research, and innovation; and advocates to ensure federal policy and programs consider the needs of both populations. ACL’s programs work together to encourage and support health, independence, and resilience throughout the lifespan and play a critical role in reducing costs of health care. ACL works closely with states, tribes, and the aging and disability networks, and, most important, with older adults and people with disabilities to ensure that ACL’s programs are tailored to the unique needs of the people they serve.
University Centers for Excellence in Developmental Disabilities Education, Research, and Services (UCEDDs), authorized under the Developmental Disabilities Assistance and Bill of Rights Act (Public Law 106-402), are a nationwide network of independent but interlinked centers, representing an expansive national resource for addressing issues, finding solutions, and advancing research related to the needs of individuals with developmental disabilities and their families. Four core functions frame the UCEDD program:
- Interdisciplinary pre-service preparation and continuing education;
- Research, including basic or applied research, evaluation, and public policy analysis;
- Information dissemination; and
- Community services, including direct services, training, technical assistance, and model demonstrations.
UCEDDs support activities that address a range of issues, from early intervention to supported employment. Additional grants may be awarded to UCEDDs to conduct national training and other initiatives. Current national training initiatives are funded to address supporting people with intellectual and developmental disabilities with co-occurring mental or behavioral health disabilities and community-based transitions. A few examples of work being done by UCEDDs are described below.
- Through the University of Maine’s Center for Community Inclusion and Disability Studies’ Interdisciplinary Disability Studies program, undergraduate and graduate students explore disability within the larger context of diversity and examine professional practice, scholarship, and policy.
- The Early Childhood Program at the University of Wisconsin-Madison’s Waisman Center offers a model supportive learning environment for a developmentally diverse group of children between the ages 1 and 5. The program takes advantage of the Waisman Center’s expertise and provides important research and training opportunities for faculty and qualified students. It also serves as a resource for early childhood professionals in the community.
- Since 1972, the Westchester Institute for Human Development has provided services in Valhalla, New York. Mitchell Levitz, who has Down syndrome, received services as a child at the Westchester Institute and became a self-advocate and staff member of the Institute as an adult. His story on how early intervention and speech therapy helped put him on a path to autonomy is told here. Mitchell retired in 2020, after close to 20 years as a staff member at the Westchester Institute.
- The MIND Institute at the University of California, Davis has been a national leader in autism research, including work on effective early interventions and studies using virtual reality technology. Lectures from MIND Institute experts are available online.
Protection and Advocacy Systems (P&As), authorized under the Developmental Disabilities Assistance and Bill of Rights Act (Public Law 106-402), empower individuals with disabilities and advocate on their behalf. There are 57 P&As in U.S. states and territories, and each is independent of service-providing agencies in their state/territory. P&As are designated by the governor and provide legal advocacy to ensure the personal and civil rights of individuals with disabilities. P&As provide legal support to traditionally unserved or underserved populations to help them navigate the legal system to achieve resolution and encourage systems change. P&As engage in legal advocacy in a wide range of areas, from assisting people in accessing needed health care or HCBS, to representing students with disabilities and their families in getting needed educational supports, and addressing disability discrimination. P&As ensure that individuals with disabilities are able to exercise their rights to make choices, contribute to society, and live independently. While their focus is most often legal, P&As also engage in a range of other efforts to promote the rights of individuals with disabilities. They often provide information and referrals, as well as training and technical assistance to service providers, state legislators, and other policymakers. P&As also conduct self-advocacy training and raise public awareness of legal and social issues affecting individuals with developmental disabilities and their families. Examples of P&A activities are described below.
- P&As across the country play a crucial role in addressing abuse and neglect of people with intellectual and developmental disabilities. For example, Disability Rights District of Columbia (DRDC) investigated the death of a 22-year-old man with intellectual and developmental disabilities. Their investigation found that being improperly restrained contributed to his death. DRDC worked with the District of Columbia Developmental Disabilities Agency to develop and implement guidelines for the safe use of restraints during crises. They worked together to improve training for residential service providers on developing and executing behavior support plans (BSPs) for residents with intellectual and developmental disabilities, including ensuring that BSPs are appropriate for the individual’s health conditions, and DRDC is monitoring to ensure ongoing compliance with the guidelines.
- P&As advocate to resolve a variety of education-related issues, including seclusion and restraint of students with disabilities and ensuring students’ access to services, supports, and other resources they need to attend school. For example, on behalf of students with disabilities who are incarcerated in state-run adult prison facilities, Disability Rights New Mexico (DRNM) filed an administrative complaint with the New Mexico Public Education Department (PED) regarding the prison system’s failure to provide legally required special education and related services. The PED’s investigation substantiated DRNM’s complaint on all grounds, finding that the adult prison facilities were non-compliant with state and federal standards of special education and requiring the facilities to take corrective action. This systemic corrective action plan will lead to greater accommodation and protection of the rights of incarcerated youth with disabilities.
- P&As support people with disabilities in finding and maintaining affordable, accessible housing in the community and addressing housing discrimination. For example, Disability Rights Kentucky (DRKY) helped a 20-year-old woman with intellectual and developmental disabilities secure safe housing in the community. The woman lived at a homeless shelter and had been financially and sexually exploited. Although she was at risk for additional abuse, she had been denied the emergency services needed to leave the shelter for stable housing. DRKY worked with her case manager to strengthen her case, ultimately helping her secure housing and the supportive services she needed.
- Employment in integrated settings, at competitive wages, is an important part of community inclusion for people with disabilities. P&As advocate both for individuals and at the system level and provide a range of services that support employment for people with intellectual and developmental disabilities. For example, Equip for Equality, the Illinois P&A, collaborated with disability advocates and community organizations to educate policymakers and provide technical assistance as both the city and state considered phasing out sub-minimum wages for people with intellectual and developmental disabilities. Ultimately, a Chicago city ordinance was proposed to include elimination of sub-minimum wages for people with disabilities in the city’s larger effort to increase wages for all workers, and the governor of Illinois issued an executive order to prohibit new State Use contracts with entities that pay sub-minimum wages. The P&A is continuing to work with the city, state, and other disability advocates on implementation, including ensuring people with intellectual and developmental disabilities who had worked in sub-minimum wage jobs are transitioned to competitive, integrated employment.
State Councils on Developmental Disabilities (SCDDs), authorized under the Developmental Disabilities Assistance and Bill of Rights Act (Public Law 106-402), are driven by people with intellectual and developmental disabilities, families, and other key stakeholders. SCDDs in each state and territory focus on developmental disabilities that are lifelong, significant, and require ongoing support, such as autism. SCDDs create partnerships, collaborations, innovative programs, and equal opportunities to improve the daily lives of people with intellectual and developmental disabilities; spark community change by bringing together people and partners to create equity in education, health, employment, and life; empower self-advocates and family leaders, influence law and policy, and educate and protect people with intellectual and developmental disabilities; and educate decision-makers using research and lived experiences to improve the lives of people with intellectual and developmental disabilities.
SCDDs are catalysts for positive change. Their work removes barriers and increases opportunities for people with intellectual and developmental disabilities so they can:
- Participate fully and live in the community;
- Become leaders and self-advocates, create their own paths, and help others;
- Access health care to live longer, healthier lives;
- Complete secondary (grades 6-12) and postsecondary (after grade 12) education;
- Find and succeed in jobs that fit their individual interests and goals;
- Stay connected and safe during emergencies and disasters; and
- Enjoy recreational and social activities.
Below are examples of SCDD activities supporting community living for people with developmental disabilities.
- Partners in Policymaking was developed by the Minnesota Governor’s Council on Developmental Disabilities in 1987 to empower people with developmental disabilities and their family members to become leaders and advocates. Since then, more than 21,000 have completed the program in the United States, and more than 2,000 have participated internationally. A self-advocate describes what the program means in this video.
- The District of Columbia Developmental Disabilities Council collaborates with local health and community-based stakeholders to incorporate the functional and accessibility needs of District of Columbia residents with developmental disabilities in emergency planning.
- Many SCDDs participate in Project SEARCH, a program which uses real-life work experience to help youth with disabilities make successful transitions from school to adult life.
- Through its Real Communities program, the Georgia Council on Developmental Disabilities brings people with and without disabilities together for projects to improve the community. This video shows the program in action.
- The Iowa Developmental Disabilities Council developed an informational campaign to help educate Iowans with intellectual and developmental disabilities about protecting themselves from COVID-19. The campaign included flyers, social media posts, radio ads, and a toolkit to help developmental disabilities network partners and other stakeholders share information. The campaign reached 800,000 Iowans with disabilities, and 99% of partner organizations that responded to the Council’s annual survey indicated that the campaign was helpful in supporting their work.
- The New York State Developmental Disabilities Council is funding a technology-based training grant called TECH Launch to help individuals with intellectual and developmental disabilities learn in-demand technology skills. Participants in this program receive career exploration mentoring services and assistance to navigate the job application process. In addition, a web- and data-based system was developed to record training certificates and help employers identify candidates with the skills needed to fill job openings.
- The Kansas Developmental Disabilities Council’s Family Employment Awareness Training is focused on helping discouraged job seekers with intellectual and developmental disabilities identify and create new employment goals. The program connects people with intellectual and developmental disabilities and their families to training and services to provide support through their journey to competitive, integrated employment. Training is provided in both English and Spanish.
- The Wyoming Governor’s Council on Developmental Disabilities commissioned a study of the adminis-tration of guardianship statutes in the courts. The study found that a guardian ad litem – an impartial official appointed to advocate for the best interests of the person for whom a guardian may be appointed – was appointed in only 102 of the state’s 256 guardianship cases. The study also found that protection of the rights of the person with intellectual and developmental disabilities varied significantly by county. Armed with these results, the Council has launched focused advocacy and outreach efforts to increase public awareness and educate state legislators and other policy makers about alternatives to guardianship and options that preserve the individual’s rights to self-determination.
- The Washington State Developmental Disabilities Council co-funded a three-year pilot project with the state’s Developmental Disabilities Administration on a project to use smart home technology solutions to provide a variety of assistance, such as reminders to take medication, support for cooking, and other assistance with activities of daily living to help people with intellectual and developmental disabilities live more independently. The project matched technology to the needs and skills of the participants. This year, a detailed evaluation is being conducted to examine the project’s impact and identify opportunities to expand and refine the initiative to meet needs across the state.
- The California State Developmental Disabilities Council has worked with public health and emergency response agencies to improve outcomes for people with intellectual and developmental disabilities in disasters and emergencies. In collaboration with the Federal Emergency Management Agency (FEMA), the American Red Cross, and the Governor’s Office of Emergency Services, the Council provided training, tools, and resources to first responders to help build their capacity to address the unique needs of people with intellectual and developmental disabilities and developed a plain language emergency response toolkit for people with intellectual and developmental disabilities. The council also provided over 6,000 emergency "go-kits" to people with intellectual and developmental disabilities to support individual emergency preparedness efforts. The kit contained essential items, such as a flashlight and first aid kit.
ACL manages the Centers for Independent Living (CILs) and Independent Living Services (ILS) programs under the Rehabilitation Act, as amended. The CIL program funds 352 awards to community-based organizations that provide independent living services to individuals with disabilities. The ILS program funds 56 states and territories to sustain, expand, and improve independent living services in each state. Together, these programs promote the independent living of individuals with disabilities to maximize the leadership, empowerment, independence, and productivity of individuals with disabilities and the integration and full inclusion of individuals with disabilities into American society by enhancing consumer control; increasing use of peer support, self-help, and self-determination; ensuring equal access; and supporting individual and system advocacy.
CILs are designed and operated by individuals with disabilities and provide independent living services for people with disabilities. CILs work to support community living and independence for people with disabilities across the nation based on the belief that all people can live with dignity, make their own choices, and participate fully in society. These programs provide tools, resources, and supports for integrating people with disabilities fully into their communities to promote equal opportunities, self-determination, and respect. At a minimum, centers funded by the program are required to provide the following independent living core services:
- Information and referral;
- Independent living skills training;
- Peer counseling;
- Individual and systems advocacy; and
- Services that facilitate transition from nursing homes and other institutions to the community, provide assistance to those at risk of entering institutions, and facilitate transition of youth to postsecondary life.
Centers also may provide, among other services:
- Psychological counseling,
- Assistance in securing housing or shelter,
- Personal assistance services,
- Transportation referral and assistance,
- Physical therapy,
- Mobility training,
- Rehabilitation technology,
- Recreation, and
- Other services necessary to improve the ability of individuals with significant disabilities to function independently in the family or community and/or to continue in employment.
Centers for Medicare & Medicaid Services (CMS)
CMS works with states to assure and improve quality in Medicaid HCBS programs to provide the opportunity for Medicaid beneficiaries to receive services in their own homes and communities. These programs serve a variety of targeted population groups, including older adults and people with intellectual and developmental disabilities (such as ASD), physical disabilities, and/or mental illnesses.
States can utilize a variety of federal authorities to design their HCBS programs, including Section 1915(c) HCBS waivers, Section 1915(i) state plan HCBS benefit, Section 1915(j) self-directed personal assistance services state plan benefit, Section 1915(k) "Community First Choice" option, and Section 1115(a) demonstrations. HCBS programs afford states a way to provide services to various targeted populations, including persons diagnosed with ASD. States may propose to provide defined populations services such as behavioral therapies, respite care, personal care, and expressive therapies. These services must supplement and not supplant state plan services, including those required under the mandatory Medicaid EPSDT benefit for children beneficiaries under the age of 21.
Services and supports that can be provided under HCBS include, but are not limited to: extended state plan services such as skilled nursing care; occupational, speech, and physical therapies; dietary management by registered dieticians; pharmaceutical services; durable medical equipment; case management including information and referral services; personal care (including dressing, bathing, toileting, eating, transferring to or from a bed or chair, etc.); and caregiver and client training. Examples of HCBS to support daily living that may be included at the option of the state include: habilitation (assistance with acquisition, retention, or improvement in self-help, socialization, and adaptive skills); home-delivered meal programs; up to two meals per day and that do not constitute a full nutritional regimen; non-medical transportation; home modifications; homemaker and chore services; remote support services; supported employment services; and adult day health. The Medicaid HCBS authorities may additionally authorize Medicaid payment of community integration activities, when linked to an assessed need of a Medicaid-eligible individual and reflected in their person-centered service plan. States determine the array of HCBS provided to targeted populations, which can include individuals diagnosed with ASD.
In September 2019, CMS initiated the HCBS Special Projects contract to advance the delivery of HCBS for specific Medicaid-eligible populations, including youth with disabilities who are transitioning out of the foster care system and adults with intellectual and developmental disabilities living with and cared for by aging parents and guardians. In addition, the contract focused on strategies to strengthen the direct service workforce furnishing HCBS under the Medicaid program. Specific activities under this contract included:
- Identifying and disseminating promising practices to improve quality of care and services and/or promote positive outcomes for youth with disabilities as they transition out of foster care and adults with intellectual and developmental disabilities who are living with and cared for by aging parents and guardians, particularly as aging parents and guardians are unable to care for their adult children with intellectual and developmental disabilities because of functional limitations, acute or chronic illness, or death;
- Convening a summit for each of these population groups, as well as on direct service workforce strategies, focused on identifying specific policy or programmatic recommendations for improving the system of care; and
- Producing and disseminating training and technical assistance products focused on these populations and the workforce serving individuals receiving HCBS.
CMS also incorporated a technical expert workgroup for each project. This contract ended in March 2023. Various resources based on learnings from this contract, including several deliverables that have not yet been finalized, will be disseminated broadly upon release.
In July 2022, CMS released the first-ever HCBS quality measure set to promote both consistent quality measurement within and across state Medicaid HCBS programs and health equity among the millions of older adults and people with disabilities who need LTSS, including individuals with autism. Further, the Ensuring Access to Medicaid Services proposed rule discussed earlier included a provision that, if finalized, would require states to report every other year on the HCBS Quality Measure Set. This proposed requirement also included phased-in requirements for states to stratify their data for certain measures by demographic and other factors in order to assess disparities and advance health equity.
Through Section 9817 of the American Rescue Plan Act of 2021, states are investing over $28 billion in activities to enhance, expand, and strengthen Medicaid HCBS, including expanding access to services and improving quality of care for individuals with autism. Of this funding, states are investing over $8 billion in a broad range of activities to enhance, expand, and strengthen Medicaid HCBS for people with intellectual and developmental disabilities, including individuals with autism. For example, states are reducing wait lists for services, expanding access to employment supports for people with intellectual and developmental disabilities, and providing specialized training to direct support professionals to improve the care provided to people with autism.
Health Homes is a Medicaid state plan optional benefit authorized under Section 1945 of the Social Security Act. Health Homes provide a comprehensive system of care coordination for qualified Medicaid beneficiaries who have two or more chronic conditions, have one chronic condition and are at risk for a second, or have one serious and persistent mental health condition. Qualifying chronic conditions listed in the Social Security Act are mental health conditions, substance use disorder, asthma, diabetes, heart disease, and overweight (body mass index [BMI] over 25); other chronic conditions, such as ASD, may be considered by CMS for approval.
Health Home providers integrate and coordinate all primary, acute, behavioral health, and LTSS to treat the "whole-person." Health Homes are responsible for coordination of both clinical and non-clinical needs of the individual and work with all the individual’s care providers to establish prevention strategies and ways to educate the individual about their condition and to support the individual in maintaining wellness and improving overall health quality. States receive a 90% enhanced match for the first eight quarters from the effective date of their state plan amendment (SPA) and their regular service match rate thereafter. More information about this program is available at the Health Home Information Resource Center.
Listed below are the six Health Home services provided under the Health Home state plan benefit:
- Comprehensive Care Management refers to the initial and ongoing assessment of an enrollee’s needs and management of services aimed at the integration of primary, acute, behavioral, and specialty health care; long term services and supports; and community support services, using a comprehensive person-centered care plan, which addresses all clinical and non-clinical needs and promotes wellness and management of chronic conditions in pursuit of optimal health outcomes.
- Care Coordination refers to facilitating access to, and the monitoring of, services identified in a person-centered care plan to manage chronic conditions for optimal health outcomes and to promote wellness.
- Health Promotion refers to the education and engagement of an individual in making decisions that promote their maximum independent living skills and lifestyle choices that achieve goals including good health, proactive management of chronic conditions, early identification of risk factors, and appropriate screening for emerging health problems.
- Comprehensive Transitional Care refers to the facilitation of services for the individual and family/ caregiver when the individual is transitioning between levels of care (including, but not limited to, hospital, nursing facility, intermediate care facility, rehabilitation facility, community-based residential setting, family, or self-care) or when an individual is electing to transition to a new Health Home provider.
- Individual and Family Supports refers to the provision of information and activities that support enrollees and the enrollee support members to maintain and promote quality of life, with particular focus on community living options.
- Referral to Community/Social Supports refers to the provision of information and assistance for the purpose of referring enrollees and enrollee support members to community-based resources that can meet the needs identified on the enrollee’s person-centered care plan.
In August 2022, CMS released guidance on a new optional Medicaid Health Home benefit authorized under Section 1945A of the Social Security Act that became available beginning on October 1, 2022. This new option helps state Medicaid programs provide Medicaid-eligible children who have medically complex conditions, including autism, with person-centered care management, care coordination, and patient and family support. This new benefit will help these children receive coordination for the care they need, including across state lines. The services provided under the new benefit include providing access to the full range of pediatric specialty and subspecialty medical services, including services from out-of-state providers, as medically necessary. States with approved Medicaid SPAs to cover the new Health Home benefit will receive an increase of 15 percentage points in federal matching for their expenditures on Health Home services during the first two FY quarters that the SPA is in effect. CMS also committed to offer ongoing technical assistance to states about implementation of the new optional benefit.
The Money Follows the Person (MFP) demonstration supports state efforts to rebalance their long-term support systems so that individuals have a choice of where they live and receive services. Since the inception of the program, more than 107,000 people with disabilities and older adults have transitioned to the community through the MFP program. Individuals with intellectual and developmental disabilities, including autism, have represented approximately 16% of MFP program participants since program inception. States have used the flexibility made available through MFP to provide HCBS to support individuals with intellectual and developmental disabilities who may have more complex and behavioral needs, including individuals with autism, so they can transition from medical institutions to community-based settings without losing access to appropriate and necessary LTSS.
Under the Consolidated Appropriations Act, 2021 (Public Law 116-260), the MFP demonstration received additional funding through FY 2023. In addition, the Consolidated Appropriations Act, 2021, expanded participant eligibility by reducing the minimum length of time that an individual needs to be in an inpatient facility before qualifying for MFP from 90 to 60 days and by allowing the days a person receives skilled nursing services or skilled rehabilitative services in a certified skilled nursing facility to be counted toward the length-of-stay requirement. These statutory changes allow more people to qualify for the program and allow people to qualify earlier in their institutional stay. The reauthorization under the Consolidated Appropriations Act, 2021, further allowed CMS to provide an opportunity for more states to participate in the program.
In addition, in August 2022, CMS awarded approximately $25 million to five states and territories not participating in the MFP demonstration to support capacity building and planning for implementation of MFP, bringing the total number of states and territories with active MFP grant awards to 41 as of November 2023. The five states and territories with capacity building and planning grants are expected to fully implement the MFP demonstration in FY 2024. The demonstration was subsequently reauthorized through FY 2027 by the Consolidated Appropriations Act, 2023 (Public Law 117-328).
CMS announced in March 2022 that it is making several changes to the scope and reimbursement rate for MFP supplemental services. MFP supplemental services have historically been defined as one-time services to support an MFP participant’s transition to the community that are otherwise not allowable under the Medicaid program. CMS notified MFP grantees that the definition of MFP supplemental services is being modified from one-time services to short-term services to support MFP participants’ transition to the community. With this change, the expanded definition of supplemental services for MFP participants now includes:
- Up to six months of short-term rental assistance and associated utility expenses to bridge the gap between when an MFP participant transitions to the community and when federal, state, or local housing assistance is secured;
- Food pantry stocking for up to a 30-day period for MFP participants;
- Payment for services and activities such as home accessibility modifications, vehicle adaptations, pre-tenancy supports, community transition services, and case management prior to an individual transitioning from an institutional setting; and
- Other costs associated with securing a community-based home that are not covered under Medicaid, such as apartment application and administrative fees.
In addition, these services are now entirely funded through MFP grants with no state share. These changes to the reimbursement rate and scope of MFP supplemental services are effective retroactively to January 1, 2022.
Department of Housing and Urban Development (HUD)
Under the Section 811 Project Rental Assistance Program (part of Section 811 Supportive Housing for Persons with Disabilities), authorized by the Frank Melville Supportive Housing Investment Act of 2010 and first implemented through a demonstration program in FY 2012, state housing agencies that have entered into partnerships with state health and human services and Medicaid agencies can apply for project rental assistance for new or existing affordable housing developments funded by Low-Income Housing Tax Credit, HOME, or other sources of funds. Under the state health care/housing agency partnership, the health care agency must develop a policy for referrals, tenant selection, and service delivery to ensure that this housing is targeted to a population most in need of deeply affordable supportive housing.
Since April 2021, HUD, alongside HHS, has provided technical assistance to help PHAs that administer Mainstream Vouchers for non-elderly persons with disabilities to strengthen their partnerships with state agencies that assist persons with disabilities to transition from institutional settings to the community.
Additionally, the Housing and Services Resource Center is part of a partnership between HUD and HHS to expand accessible, affordable housing; help people exit homelessness; improve HCBS; and address the institutional bias in America's long-term care system. The Center was created for people who work in the organizations and systems that provide housing resources and homelessness services, behavioral and mental health services, independent living services and other supportive services, and others who are working to help people live successfully and stably in the community. The goal of the Center is to foster collaboration and cross-sector partnerships, in order to streamline access to services, better leverage resources, and ultimately make community living possible for more people. People can use the Housing and Services Resource Center website to:
- Learn about how to develop and expand partnerships;
- Quickly find tools designed for community collaborations;
- Increase knowledge to support people with disabilities, older adults, and people experiencing homelessness to get and/or keep affordable and accessible housing and voluntary services; and
- Discover innovative models and strategies.
On November 1, 2023, HHS and HUD announced the launch of the Housing and Services Partnership Accelerator, which will support states in developing or expanding innovative housing-related supports and services for Medicaid-eligible people with disabilities and older adults who are experiencing or at risk of homelessness. The Partnership Accelerator is a technical assistance opportunity that will focus on helping states improve collaboration and coordination between organizations and systems that provide services and resources that help people find – and keep – stable housing in the community.
Department of Labor (DOL)
ODEP’s National Center on Leadership for the Employment and Economic Advancement of People with Disabilities (LEAD Center) supports state-level efforts to drive Employment First policies and practices. The LEAD Center also releases related resources to help bolster and enhance the delivery of long-term supports and services, including services used by people with intellectual and developmental disabilities. In 2021, the LEAD Center released a report on Increasing Access and Equity within the Workforce Development Systems Run by the States. The report examined the use of and access to services provided by the American Job Centers, which receive federal funding from DOL under the WIOA.
Medicaid HCBS programs run by states frequently include employment and work readiness supports as eligible services. These services can help autistic people and other people with developmental disabilities to attain and maintain jobs and career paths that fit interests, skills, strengths, and talents. Common employment services provided through HCBS programs include job coaches, supported employment services, career planning services, and vocational assessments.
Autistic adults also often access VR services run by states to support their employment outcomes. ODEP’s 2023 REYAAS report on VR characteristics, service use, and employment outcomes found that transition age youth and young adults account for the largest group of autistic recipients of state VR users. Between 2017 and 2019, autistic people represented about 14% (81,616) of all young adults with disabilities who applied for state VR services (566,367).
Prior studies have found significant interstate variation in VR service use and outcomes for transition age autistic youth and young adults. One study found significant interstate differences for autistic clients who received services, entered VR services during secondary school, developed timely employment plans, and secured employment at VR case exit.78 Another study identified five classes of states with distinct patterns of performance of VR service systems for autistic clients across four key indicators. These indicators included service receipt, early reach, timely services, and employment rates. About one fourth of the states had a high probability of membership in the class of states with above average performance on all four indicators for VR services.79
These findings are supported by the 2023 REYAAS report, which also found that referral sources, service experiences, and outcomes for autistic clients varied widely by state. In most states, elementary and secondary schools served as the most common referral source for VR services access by clients on the autism spectrum. However, autistic clients in four states were more likely to refer themselves than to be referred by their schools. The reason for this difference has remained unclear.
Likewise, access barriers to employment for VR clients on the autism spectrum varied widely by state. For instance, the 2023 REYAAS report found that the share of autistic clients in state VR systems who identified low income as a key barrier to employment ranged widely from 21% to 82%. Upon accessing VR services provided by states, employment outcomes for autistic youth and young adults with signed IPEs also varied widely by state. The percentage of autistic youth and young adults who exited VR services with employment ranged from 27% to 68% across the 50 states and the District of Columbia.
The 2023 REYAAS report further identified the most common VR services accessed and used by autistic clients with signed IPEs. These services included counseling and guidance, vocational assessments, job search assistance, and job placement assistance. Autistic clients of state VR services also frequently accessed pre-employment transition services, including job exploration counseling, workplace readiness training, and work-based learning experiences.
Implementation of the IACC Strategic Plan
This portion of the report covers Section 399DD(a)(2)(I) of the Public Health Service Act, as amended by the Autism CARES Act of 2019, which requires: (I) "A description of the actions taken to implement and the progress made on implementation of the strategic plan developed by the Interagency Autism Coordinating Committee."
The IACC Strategic Plan was developed by the IACC, which is a diverse committee comprising federal officials and public members representing various community perspectives. The Plan incorporates public input gathered by the Committee to prioritize areas relevant to individuals on the autism spectrum and their families, building on the latest advances in autism research and services. While federal agencies are major funders of autism research and services in the United States, the IACC also acknowledges the vital contributions of private organizations in the national autism effort.
The IACC Strategic Plan serves as a blueprint not only for guiding federal agencies but also for fostering partnerships and collaborations with private and community organizations. It aims to enhance both federal and non-federal autism activities, ensuring a collective effort to address autism-related challenges. The Recommendations/Objectives within the Plan target not only federal agencies by also non-federal private organizations that significantly contribute to autism efforts across the country.
To monitor progress, the IACC tracks contributions from both federal agencies and private organizations toward achieving the Strategic Plan’s Recommendations/Objectives. This comprehensive approach ensures a united effort in advancing autism research and services for the benefit of autistic individuals and their families.
The IACC Strategic Plan describes priorities for autism research, services, and policy and organizes them into a set of seven community-based Question areas:
- Question 1 (Screening and Diagnosis),
- Question 2 (Biology),
- Question 3 (Genetic and Environmental Factors),
- Question 4 (Interventions),
- Question 5 (Services and Supports),
- Question 6 (Lifespan), and
- Question 7 (Infrastructure and Prevalence).
All federal agencies featured in this report are making contributions toward the implementation of priorities and recommendations in the IACC Strategic Plan. Table 27 summarizes the Question areas that are addressed by both research and services activities funded by each of the departments and agencies listed in this report. Details on the relevant research and services activities of each department and agency are provided in the Autism Progress and Expenditures section of this report.
Table 27: Research (including autism-specific and disability research that may benefit individuals with autism) and autism and disability services activities of federal agencies that contribute to implementation of the IACC Strategic Plan.
| Federal Involvement in the Implementation of the IACC Strategic Plan, by Department/Agency | |||||||
|---|---|---|---|---|---|---|---|
| Department/Agency | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 |
Department/AgencyHHS ACF |
Q1✔ |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6 |
Q7 |
Department/AgencyHHS ACL |
Q1 |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyHHS ASPR |
Q1 |
Q2 |
Q3 |
Q4 |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyHHS AHRQ |
Q1✔ |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6 |
Q7✔ |
Department/AgencyHHS CDC |
Q1✔ |
Q2✔ |
Q3✔ |
Q4✔ |
Q5✔ |
Q6✔ |
Q7✔ |
Department/AgencyHHS CMS |
Q1 |
Q2 |
Q3 |
Q4 |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyHHS FDA |
Q1✔ |
Q2✔ |
Q3 |
Q4✔ |
Q5 |
Q6 |
Q7 |
Department/AgencyHHS HRSA |
Q1✔ |
Q2✔ |
Q3✔ |
Q4✔ |
Q5✔ |
Q6✔ |
Q7✔ |
Department/AgencyHHS ASPE |
Q1 |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7✔ |
Department/AgencyHHS IHS |
Q1 |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6 |
Q7 |
Department/AgencyHHS NIH |
Q1✔ |
Q2✔ |
Q3✔ |
Q4✔ |
Q5✔ |
Q6✔ |
Q7✔ |
Department/AgencyHHS SAMHSA |
Q1 |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyDoD-Army |
Q1 |
Q2✔ |
Q3✔ |
Q4✔ |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyDoD MHS/TRICARE |
Q1 |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6 |
Q7 |
Department/AgencyDoD DARPA |
Q1✔ |
Q2 |
Q3 |
Q4 |
Q5 |
Q6 |
Q7 |
Department/AgencyED |
Q1✔ |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7✔ |
Department/AgencyHUD |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6✔ |
Q7 |
Department/AgencyDOJ |
Q1 |
Q2 |
Q3 |
Q4 |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyDOL |
Q1 |
Q2 |
Q3 |
Q4 |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyDOT |
Q1 |
Q2 |
Q3 |
Q4 |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyVA |
Q1 |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyEPA |
Q1 |
Q2 |
Q3✔ |
Q4 |
Q5 |
Q6 |
Q7 |
Department/AgencyIMLS |
Q1 |
Q2 |
Q3 |
Q4 |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyNASA |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6✔ |
Q7 |
Department/AgencyNEA |
Q1 |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyNSF |
Q1✔ |
Q2✔ |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7✔ |
Department/AgencySSA |
Q1 |
Q2 |
Q3 |
Q4 |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyUSAID |
Q1✔ |
Q2 |
Q3 |
Q4✔ |
Q5✔ |
Q6✔ |
Q7 |
Department/AgencyUSGS |
Q1 |
Q2 |
Q3 |
Q4 |
Q5 |
Q6✔ |
Q7 |
As shown in Table 27, federal departments and agencies are supporting programming across all seven Question areas of the IACC Strategic Plan. All 22 topical Recommendations/Objectives and the Cross-Cutting Recommendation/Objective on girls/women found in the 2016-2017 IACC Strategic Plan, as well as the Cross-Cutting Recommendation/Objective on DEIA, are addressed by federal autism research activities (Table 28 in Appendix II). The new Cross-Cutting Recommendation on DEIA that was created for and added to the 2021-2023 IACC Strategic Plan, which covered an area that was already being tracked starting in the 2017-2018 IACC Portfolio Analysis Report, will now be tracked as a formal Recommendation; many federal agencies have been supporting activities in this area. In addition to the information in the Autism Progress and Expenditures section of this report regarding federal programs and activities that address Recommendations in the IACC Strategic Plan, the IACC ARD provides detailed information on both federally funded and privately funded research projects that address each of the IACC Strategic Plan Recommendations/Objectives.
The Budget Recommendation of the IACC Strategic Plan conveys the IACC’s recommendation for autism research funding across U.S. federal and private funders. The 2016-2017 IACC Strategic Plan called for total federal and private autism research funding to reach $685 million by 2020. According to the upcoming 2019-2020 IACC Portfolio Analysis Report, combined federal and private autism research funding for 2020 was estimated to be $418 million, with federal funding accounting for almost 83% of the total at $346 million. While total research funding was below the target of $685 million, the overall trend since 2016 has been one of growth, and 2020 autism research funding was approximately 15% higher compared to 2016 ($364 million).
Based on research funding amounts tracked over the past several years and current research needs and opportunities, in the 2021-2023 IACC Strategic Plan, the IACC recommended that federal and private funders of autism research collectively invest $685 million in autism research by 2025. This would allow for the rapid growth of research in many of the promising, emerging, and needed areas identified in the IACC Strategic Plan. To achieve this, the IACC acknowledged that new private funders and innovative funding mechanisms may be needed to support such growth. The Budget Recommendation also identified three specific high-priority research areas that could greatly benefit from targeted funding increases:
- Lifespan issues: Increased funding is needed in research on issues that are relevant to autistic adults, such as transition to adulthood, higher education, employment, housing, health care, life-long learning, service, and support opportunities, community integration, and healthy aging.
- Evidence-based interventions and services: Increasing the evidence base for new and existing interventions and services will provide additional guidance to autistic individuals and their families as they seek solutions to maximize positive outcomes.
- Research on disparities and development of culturally responsive tools and services: Continued investment is needed to close the existing gaps in outcome measures due to differences across race/ethnicity/culture, sex/gender, sexual orientation, geographic location, and socioeconomic status.
Continued robust support for autism research by federal and private funders will be needed to meet the new IACC Budget Recommendation and the need for the development of more efficient and effective tools and services to help people on the autism spectrum achieve their full potential.